Monday Poster Session
Category: Biliary/Pancreas
P1889 - Hemorrhagic Cholecystitis: An Atypical Presentation of Acute Cholecystitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- MK
Muhammad Taha Khan, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Taha Khan, MD1, Apurva Shrigiriwar, MD1, Amir Rumman, MD2
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Hemorrhagic cholecystitis (HC) is an extremely rare entity of abdominal pain that can present as a complication of cholecystitis, trauma, malignancy, and bleeding diathesis. Prompt evaluation and intervention are required in these patients as timely surgical intervention can be lifesaving. Here, we describe a case of HC with initially unrevealing workup, complicating diagnosis.
Case Description/Methods: A 62-year-old male with CML, CAD, metastatic lung adenocarcinoma, and malignant ascites presented with a month-long history of abdominal pain, nausea, and vomiting. Initial workup for acute cholecystitis and alternate biliary pathology was unrevealing, and he was managed conservatively with IV fluids and antibiotics.
A week into his hospitalization, he experienced worsening abdominal pain and difficulty tolerating oral intake. Lab work indicated a notable escalation in liver enzyme levels, accompanied by a twofold increase in total bilirubin (predominantly conjugated) raising suspicion for a Drug induced Liver Injury, leading to cessation of all hepatotoxic medications. Repeat imaging was obtained due to consistently worsening LFTs, which now revealed a distended gallbladder with sludge, wall thickening, and bile duct dilation.
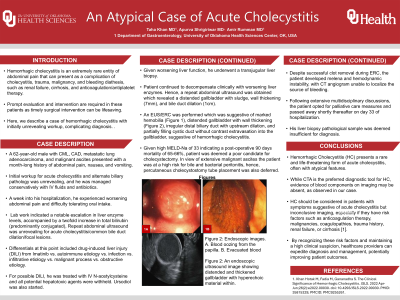
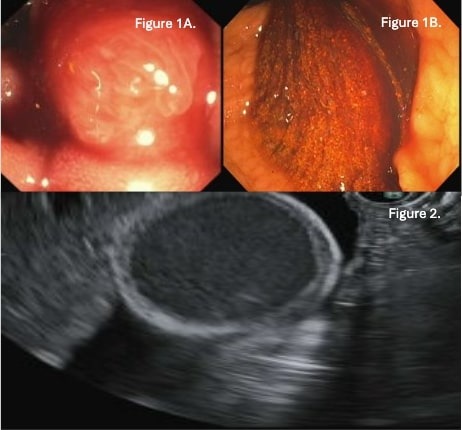
An EUS/ERC was performed which was suggestive of marked hemobilia, irregular distal biliary duct with upstream dilation, and partially filling cystic duct without contrast extravasation into the gallbladder, suggestive of hemorrhagic cholecystitis.
Given the patient's elevated surgical risk, procedures such as Cholecystostomy and Cholecystectomy were deferred. Despite successful clot removal during ERC, the patient developed melena and hemodynamic instability, with CTA unable to localize the source of bleeding.
After extensive multidisciplinary discussions, the patient opted for palliative care measures and passed away shortly thereafter.
Discussion: Hemorrhagic Cholecystitis presents a rare and life-threatening form of acute cholecystitis, often with atypical features. While CTA is the preferred diagnostic tool for HC, evidence of blood components on imaging may be absent, as observed in our case.
HC should be considered in patients with symptoms suggestive of acute cholecystitis but inconclusive imaging, especially if they have risk factors such as anticoagulation therapy, malignancies, coagulopathies, trauma history, renal failure, or cirrhosis. By recognizing these risk factors, providers can expedite diagnosis and management, potentially improving patient outcomes.
Disclosures:
Taha Khan, MD1, Apurva Shrigiriwar, MD1, Amir Rumman, MD2. P1889 - Hemorrhagic Cholecystitis: An Atypical Presentation of Acute Cholecystitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Hemorrhagic cholecystitis (HC) is an extremely rare entity of abdominal pain that can present as a complication of cholecystitis, trauma, malignancy, and bleeding diathesis. Prompt evaluation and intervention are required in these patients as timely surgical intervention can be lifesaving. Here, we describe a case of HC with initially unrevealing workup, complicating diagnosis.
Case Description/Methods: A 62-year-old male with CML, CAD, metastatic lung adenocarcinoma, and malignant ascites presented with a month-long history of abdominal pain, nausea, and vomiting. Initial workup for acute cholecystitis and alternate biliary pathology was unrevealing, and he was managed conservatively with IV fluids and antibiotics.
A week into his hospitalization, he experienced worsening abdominal pain and difficulty tolerating oral intake. Lab work indicated a notable escalation in liver enzyme levels, accompanied by a twofold increase in total bilirubin (predominantly conjugated) raising suspicion for a Drug induced Liver Injury, leading to cessation of all hepatotoxic medications. Repeat imaging was obtained due to consistently worsening LFTs, which now revealed a distended gallbladder with sludge, wall thickening, and bile duct dilation.
An EUS/ERC was performed which was suggestive of marked hemobilia, irregular distal biliary duct with upstream dilation, and partially filling cystic duct without contrast extravasation into the gallbladder, suggestive of hemorrhagic cholecystitis.
Given the patient's elevated surgical risk, procedures such as Cholecystostomy and Cholecystectomy were deferred. Despite successful clot removal during ERC, the patient developed melena and hemodynamic instability, with CTA unable to localize the source of bleeding.
After extensive multidisciplinary discussions, the patient opted for palliative care measures and passed away shortly thereafter.
Discussion: Hemorrhagic Cholecystitis presents a rare and life-threatening form of acute cholecystitis, often with atypical features. While CTA is the preferred diagnostic tool for HC, evidence of blood components on imaging may be absent, as observed in our case.
HC should be considered in patients with symptoms suggestive of acute cholecystitis but inconclusive imaging, especially if they have risk factors such as anticoagulation therapy, malignancies, coagulopathies, trauma history, renal failure, or cirrhosis. By recognizing these risk factors, providers can expedite diagnosis and management, potentially improving patient outcomes.
Figure: Figure 1: Endoscopic images. A. Blood oozing from the papilla. B. Evacuated blood
Figure 2: An endoscopic ultrasound image showing distended and thickened gallbladder with hyperechoic material within.
Figure 2: An endoscopic ultrasound image showing distended and thickened gallbladder with hyperechoic material within.
Disclosures:
Taha Khan indicated no relevant financial relationships.
Apurva Shrigiriwar indicated no relevant financial relationships.
Amir Rumman indicated no relevant financial relationships.
Taha Khan, MD1, Apurva Shrigiriwar, MD1, Amir Rumman, MD2. P1889 - Hemorrhagic Cholecystitis: An Atypical Presentation of Acute Cholecystitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
