Monday Poster Session
Category: Biliary/Pancreas
P1890 - A Rare Case of Tacrolimus-Associated Acute Pancreatitis in a Liver Transplant Recipient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arjun Chatterjee, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Zurabi Zaalishvili, MD, Rupayan Kundu, MD, Arjun Chatterjee, MD, Shreya Sengupta, MD, Shilpa Junna, MD, Syed Mohiuddin, MD
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Tacrolimus-associated acute pancreatitis (TAP) is a rare condition that requires extensive work-up with exclusion of more common causes of acute pancreatitis (AP), followed by modification of tacrolimus dosing and adjustment of goal tacrolimus trough levels. We describe a rare case of TAP in a liver transplant patient.
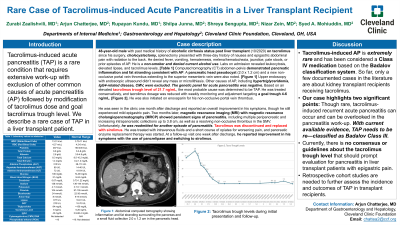
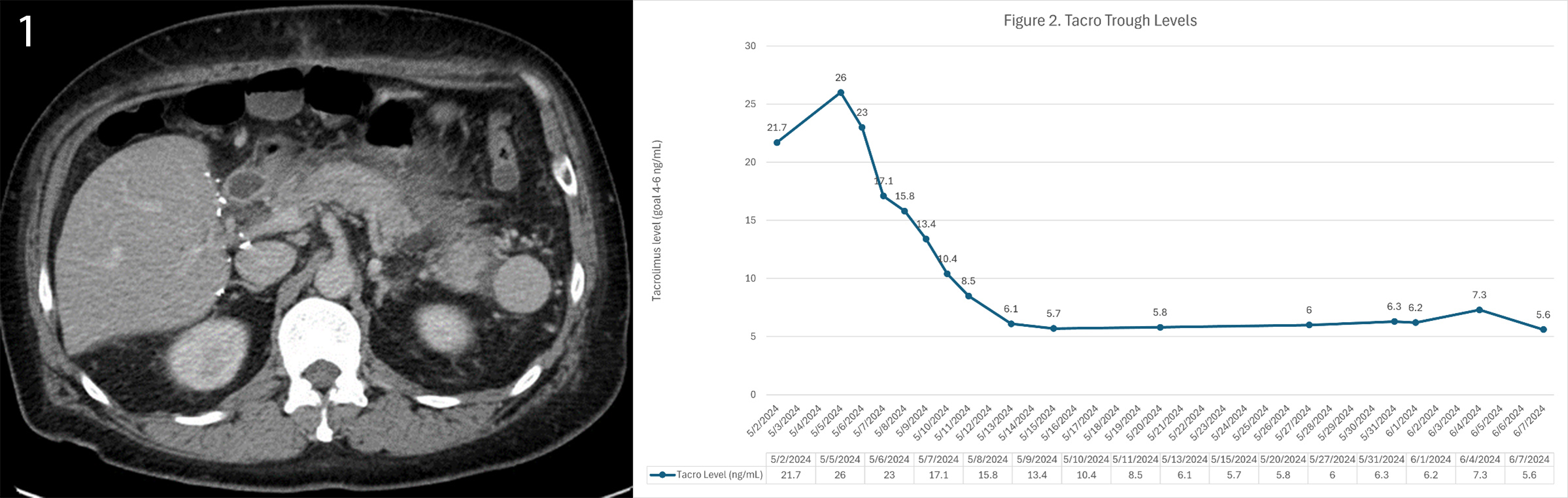
Case Description/Methods: A 48-year-old male with a past medical history of alcohol associated cirrhosis status post liver transplant three years prior presented with a three-day history of nausea and epigastric pain with radiation to the back. He denied fever, vomiting, hematemesis, melena, hematochezia, jaundice, pale stools, or prior episodes of AP. He is a non-smoker and denied current alcohol use. Labs on admission revealed leukocytosis, elevated lipase, undetectable alcohol metabolites, and elevated tacrolimus levels [Table 1]. CT abdomen-pelvis with contrast demonstrated pancreatic inflammation and fat stranding consistent with AP. A new pancreatic head pseudocyst (2.0 x 1.2 cm) and a non-occlusive portal vein thrombus extending to the superior mesenteric vein were also noted [Figure 1]. Upper endoscopy with endoscopic ultrasound didn’t reveal any pancreatic mass or microlithiasis as the cause of pancreatitis. Other causes of AP, including hypertriglyceridemia, IgG4-related disease, CMV, were excluded. Based on an elevated tacrolimus trough level of 21.7 ng/mL, the most probable cause was determined to be TAP. He was treated conservatively, and tacrolimus dosage was reduced with weekly monitoring and adjustment targeting a goal trough of 4-6 ng/mL [Figure 2].
Discussion: Tacrolimus-induced AP is extremely rare and has been considered a Class IV medication based on the Badalov classification system. So far, the only documented cases in the literature pertain to kidney transplant recipients receiving tacrolimus. Our case highlights two major points. Though rare, tacrolimus-associated recurrent acute pancreatitis can occur and can be overlooked in the pancreatitis work-up. Now with current available evidence, TAP needs to be reclassified as Badalov Class III. Currently there is no consensus or guidelines about the tacrolimus trough level that should prompt evaluation for pancreatitis in liver transplant patients with epigastric pain. Retrospective cohort studies are needed to further assess the incidence and outcomes of TAP in transplant recipients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zurabi Zaalishvili, MD, Rupayan Kundu, MD, Arjun Chatterjee, MD, Shreya Sengupta, MD, Shilpa Junna, MD, Syed Mohiuddin, MD. P1890 - A Rare Case of Tacrolimus-Associated Acute Pancreatitis in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Tacrolimus-associated acute pancreatitis (TAP) is a rare condition that requires extensive work-up with exclusion of more common causes of acute pancreatitis (AP), followed by modification of tacrolimus dosing and adjustment of goal tacrolimus trough levels. We describe a rare case of TAP in a liver transplant patient.
Case Description/Methods: A 48-year-old male with a past medical history of alcohol associated cirrhosis status post liver transplant three years prior presented with a three-day history of nausea and epigastric pain with radiation to the back. He denied fever, vomiting, hematemesis, melena, hematochezia, jaundice, pale stools, or prior episodes of AP. He is a non-smoker and denied current alcohol use. Labs on admission revealed leukocytosis, elevated lipase, undetectable alcohol metabolites, and elevated tacrolimus levels [Table 1]. CT abdomen-pelvis with contrast demonstrated pancreatic inflammation and fat stranding consistent with AP. A new pancreatic head pseudocyst (2.0 x 1.2 cm) and a non-occlusive portal vein thrombus extending to the superior mesenteric vein were also noted [Figure 1]. Upper endoscopy with endoscopic ultrasound didn’t reveal any pancreatic mass or microlithiasis as the cause of pancreatitis. Other causes of AP, including hypertriglyceridemia, IgG4-related disease, CMV, were excluded. Based on an elevated tacrolimus trough level of 21.7 ng/mL, the most probable cause was determined to be TAP. He was treated conservatively, and tacrolimus dosage was reduced with weekly monitoring and adjustment targeting a goal trough of 4-6 ng/mL [Figure 2].
Discussion: Tacrolimus-induced AP is extremely rare and has been considered a Class IV medication based on the Badalov classification system. So far, the only documented cases in the literature pertain to kidney transplant recipients receiving tacrolimus. Our case highlights two major points. Though rare, tacrolimus-associated recurrent acute pancreatitis can occur and can be overlooked in the pancreatitis work-up. Now with current available evidence, TAP needs to be reclassified as Badalov Class III. Currently there is no consensus or guidelines about the tacrolimus trough level that should prompt evaluation for pancreatitis in liver transplant patients with epigastric pain. Retrospective cohort studies are needed to further assess the incidence and outcomes of TAP in transplant recipients.
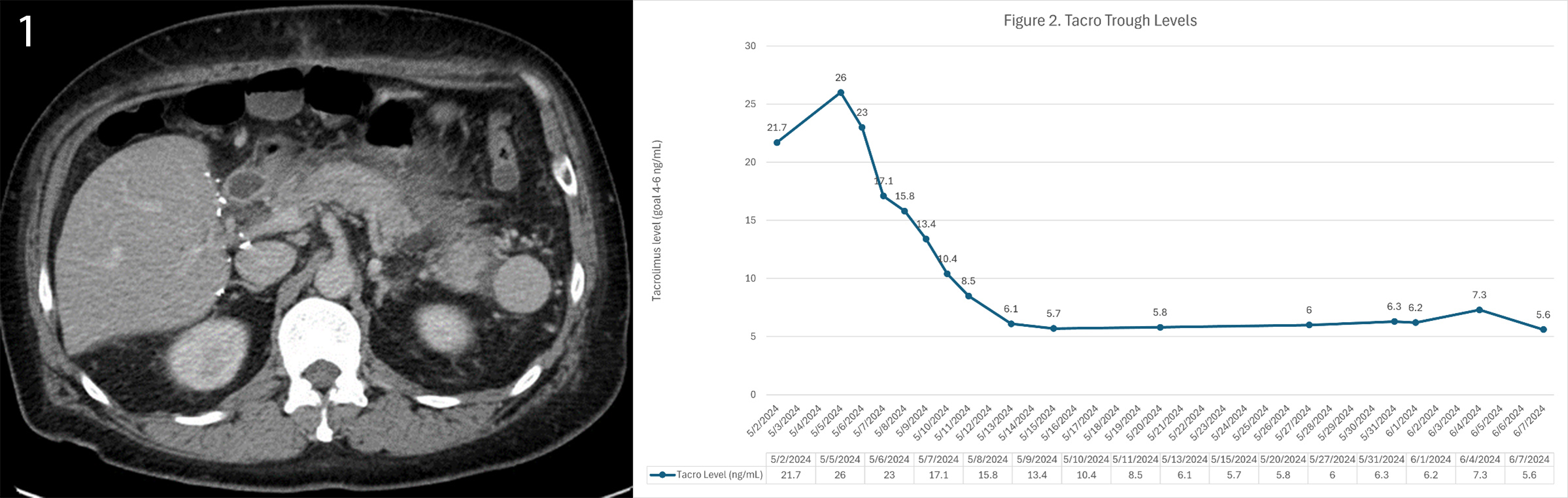
Figure: Figure 1: Abdominal computed tomography showing inflammation and fat stranding surrounding the pancreas and a small fluid collection 2.0 x 1.2 cm in the pancreatic head. Figure 2: Tacrolimus trough levels during initial presentation and follow-up.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zurabi Zaalishvili indicated no relevant financial relationships.
Rupayan Kundu indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Shreya Sengupta indicated no relevant financial relationships.
Shilpa Junna indicated no relevant financial relationships.
Syed Mohiuddin indicated no relevant financial relationships.
Zurabi Zaalishvili, MD, Rupayan Kundu, MD, Arjun Chatterjee, MD, Shreya Sengupta, MD, Shilpa Junna, MD, Syed Mohiuddin, MD. P1890 - A Rare Case of Tacrolimus-Associated Acute Pancreatitis in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
