Monday Poster Session
Category: Biliary/Pancreas
P1893 - A Case of Atraumatic Splenic Rupture in Chronic Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shriya Vudari, MD
Willis Knighton Health System
Shreveport, LA
Presenting Author(s)
Shriya Vudari, MD, Prajwal Kumsi Sreedhar, MD, Brian Monaco, MD
Willis Knighton Health System, Shreveport, LA
Introduction: Atraumatic splenic rupture is a life-threatening complication rarely seen in patients with chronic pancreatitis. While the mechanism remains poorly understood, the pathophysiology is linked to the anatomical proximity between the pancreatic tail and spleen during the inflammatory process. Splenic complications may manifest during active or chronic pancreatitis, presenting as isolated splenic vein thrombosis, intrasplenic pseudocysts, splenic rupture, infarction, necrosis, or splenic hematoma. This case underscores the significance of considering a broad range of differentials and the timely intervention necessary to avert fatal outcomes.
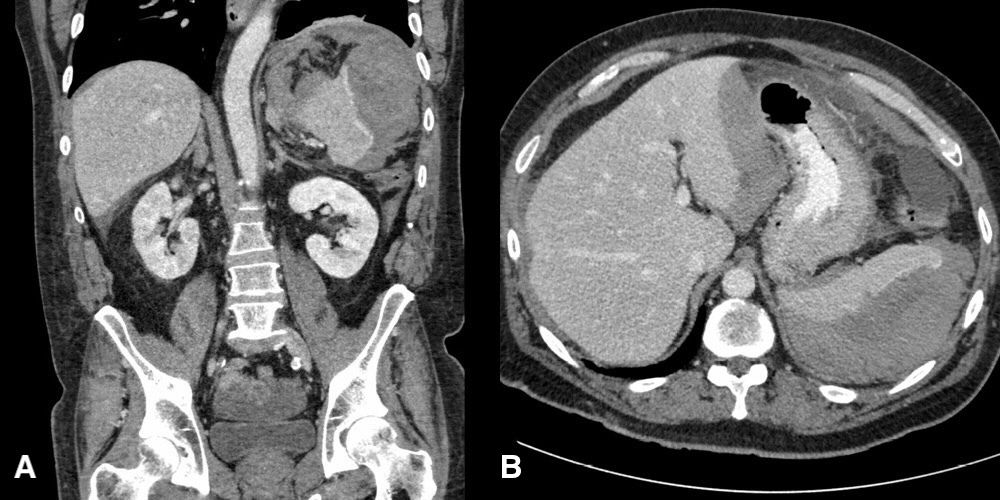
Case Description/Methods: A 47-year-old male with a history of chronic tobacco and alcohol abuse presented with sudden onset abdominal pain, nausea, and vomiting. Presenting labs showed a total bilirubin of 3.3 mg/dL with normal transaminases and an elevated lipase at 1088 U/L. Hemoglobin/hematocrit and coagulation panel were within normal limits. CT abdomen showed changes of chronic pancreatitis but also incidentally revealed a grade 3 splenic laceration accompanied by a large subcapsular splenic hematoma rupture. Soon after, the patient was noted to have a significant drop in hemoglobin prompting emergent transfer to the ICU for close hemodynamic monitoring. Consultations with relevant specialties were initiated, ultimately leading to the patient undergoing embolization of multiple splenic branches by interventional radiology.
Discussion: The etiology of spontaneous splenic hematoma in chronic pancreatitis remains speculative, with one hypothesis suggesting the propagation of inflammation to the splenic hilum, leading to pancreatic enzyme erosion of the capsule and subsequent damage. The selection of nonoperative, operative, or embolization approaches hinges upon the patient's hemodynamic status, imaging findings, and the clinical judgment of the managing team. Given the potential for rapid deterioration, prompt diagnosis and appropriate management can significantly impact the morbidity and mortality associated with splenic rupture. Maintaining a high index of clinical suspicion and enhancing awareness of the pathophysiology and presentation of splenic complications in pancreatitis can help physicians identify these critical complications early on.
Disclosures:
Shriya Vudari, MD, Prajwal Kumsi Sreedhar, MD, Brian Monaco, MD. P1893 - A Case of Atraumatic Splenic Rupture in Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Willis Knighton Health System, Shreveport, LA
Introduction: Atraumatic splenic rupture is a life-threatening complication rarely seen in patients with chronic pancreatitis. While the mechanism remains poorly understood, the pathophysiology is linked to the anatomical proximity between the pancreatic tail and spleen during the inflammatory process. Splenic complications may manifest during active or chronic pancreatitis, presenting as isolated splenic vein thrombosis, intrasplenic pseudocysts, splenic rupture, infarction, necrosis, or splenic hematoma. This case underscores the significance of considering a broad range of differentials and the timely intervention necessary to avert fatal outcomes.
Case Description/Methods: A 47-year-old male with a history of chronic tobacco and alcohol abuse presented with sudden onset abdominal pain, nausea, and vomiting. Presenting labs showed a total bilirubin of 3.3 mg/dL with normal transaminases and an elevated lipase at 1088 U/L. Hemoglobin/hematocrit and coagulation panel were within normal limits. CT abdomen showed changes of chronic pancreatitis but also incidentally revealed a grade 3 splenic laceration accompanied by a large subcapsular splenic hematoma rupture. Soon after, the patient was noted to have a significant drop in hemoglobin prompting emergent transfer to the ICU for close hemodynamic monitoring. Consultations with relevant specialties were initiated, ultimately leading to the patient undergoing embolization of multiple splenic branches by interventional radiology.
Discussion: The etiology of spontaneous splenic hematoma in chronic pancreatitis remains speculative, with one hypothesis suggesting the propagation of inflammation to the splenic hilum, leading to pancreatic enzyme erosion of the capsule and subsequent damage. The selection of nonoperative, operative, or embolization approaches hinges upon the patient's hemodynamic status, imaging findings, and the clinical judgment of the managing team. Given the potential for rapid deterioration, prompt diagnosis and appropriate management can significantly impact the morbidity and mortality associated with splenic rupture. Maintaining a high index of clinical suspicion and enhancing awareness of the pathophysiology and presentation of splenic complications in pancreatitis can help physicians identify these critical complications early on.
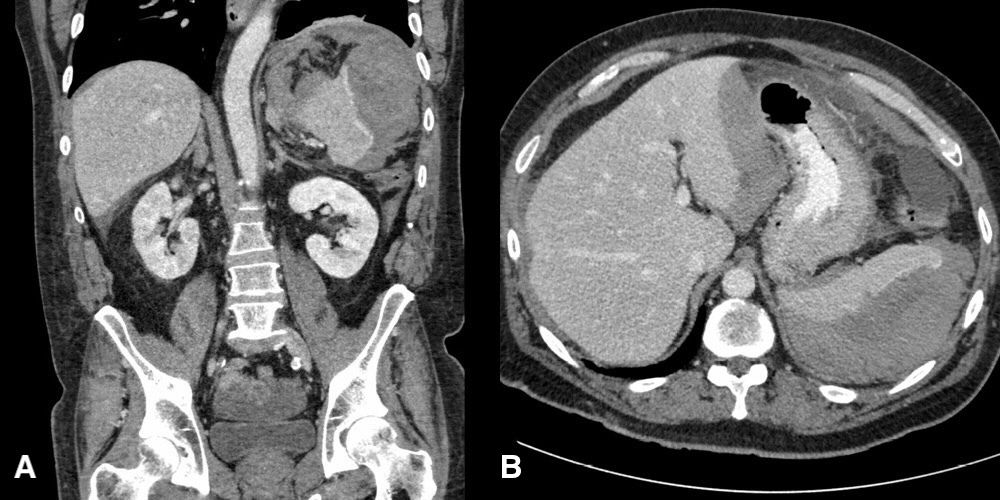
Figure: Figure 1. (A-B) showing Grade-3 splenic laceration with moderate to large-sized ruptured subcapsular splenic hematoma.
Disclosures:
Shriya Vudari indicated no relevant financial relationships.
Prajwal Kumsi Sreedhar indicated no relevant financial relationships.
Brian Monaco indicated no relevant financial relationships.
Shriya Vudari, MD, Prajwal Kumsi Sreedhar, MD, Brian Monaco, MD. P1893 - A Case of Atraumatic Splenic Rupture in Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
