Monday Poster Session
Category: Biliary/Pancreas
P1898 - Acute Pancreatitis in the Setting of Vaso-Occlusive Sickle Cell Crisis: A Rare Etiology
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gabriela Mendez, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Gabriela Mendez, MD, Laura Fernandez, MD, Marwah Farooqui, DO, John Pueringer, DO, Abdullah Memon, MD
University of Illinois College of Medicine, Chicago, IL
Introduction: Sickle cell disease (SCD) is an autosomal recessive disorder of the β-globin chain of hemoglobin that leads to extensive red cell sickling, resulting in painful vaso-occlusive crises (VOC). Typically, the spleen is the most affected organ in the gastrointestinal tract, however, more rarely, acute pancreatitis (AP) develops from microvascular occlusion and ischemic injury. We present the case of a 22-year-old male patient who had multiple admissions for AP as a result VOC episodes.
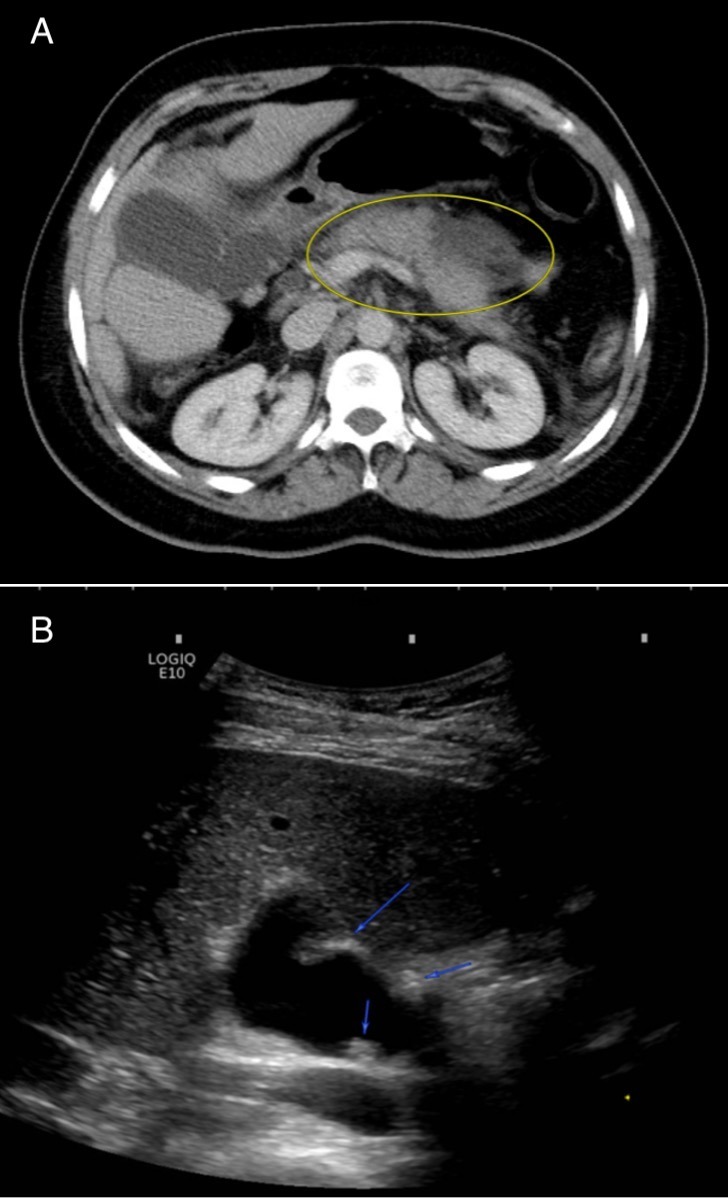
Case Description/Methods: A 22-year-old male with medical history of SCD and primary sclerosing cholangitis was admitted for acute severe epigastric pain, nausea, and vomiting. Laboratories were remarkable for elevated lipase 1,085 U/L, triglycerides 68 mg/dL and calcium 10.0 mg/dL. IgG4 levels were unrevealing. Abdominal CT scan with IV contrast showed edematous enlargement of the pancreas, peripancreatic fat stranding, and free fluid, consistent with AP. There was no cholelithiasis. The patient denied recent alcohol or steroid use. Symptom management included intravenous fluids (IVF) and pain medications. Five months later, the patient returned to the emergency department with a similar presentation of severe epigastric abdominal pain and back pain which he related to his typical VOC. This time, there was significantly elevated lipase 8,265 U/L. Right upper quadrant US (RUQUS) revealed cholelithiasis but no choledocholithiasis. Treatment for AP included IVF and pain medications. Seven months later, he was admitted for recurrent AP. Lipase was 7,037 U/L and RUQUS showed intraluminal gallbladder polyps but no cholelithiasis (Figure B). After ruling out all the common etiologies of AP including gallstones, ethanol use, hypertriglyceridemia, steroid use, and autoimmunity, the etiology of recurrent episodes of acute pancreatitis was presumably to be secondary to VOC.
Discussion: Vaso-occlusive crises can present as acute sharp abdominal pain from micro-occlusive infarcts of the mesentery and abdominal viscera. The clinical presentation may be indistinguishable from other acute intra-abdominal disease processes, like cholecystitis, splenic sequestration, and appendicitis. Vaso-occlusive-induced pancreatitis is not common but is possibly underreported as the diagnosis can be challenging and difficult to differentiate from usual pain crises. Our case illustrates the need to include vaso-occlusive-induced pancreatitis on the list of differential diagnoses when treating patients with SCD and abdominal pain.
Disclosures:
Gabriela Mendez, MD, Laura Fernandez, MD, Marwah Farooqui, DO, John Pueringer, DO, Abdullah Memon, MD. P1898 - Acute Pancreatitis in the Setting of Vaso-Occlusive Sickle Cell Crisis: A Rare Etiology, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Illinois College of Medicine, Chicago, IL
Introduction: Sickle cell disease (SCD) is an autosomal recessive disorder of the β-globin chain of hemoglobin that leads to extensive red cell sickling, resulting in painful vaso-occlusive crises (VOC). Typically, the spleen is the most affected organ in the gastrointestinal tract, however, more rarely, acute pancreatitis (AP) develops from microvascular occlusion and ischemic injury. We present the case of a 22-year-old male patient who had multiple admissions for AP as a result VOC episodes.
Case Description/Methods: A 22-year-old male with medical history of SCD and primary sclerosing cholangitis was admitted for acute severe epigastric pain, nausea, and vomiting. Laboratories were remarkable for elevated lipase 1,085 U/L, triglycerides 68 mg/dL and calcium 10.0 mg/dL. IgG4 levels were unrevealing. Abdominal CT scan with IV contrast showed edematous enlargement of the pancreas, peripancreatic fat stranding, and free fluid, consistent with AP. There was no cholelithiasis. The patient denied recent alcohol or steroid use. Symptom management included intravenous fluids (IVF) and pain medications. Five months later, the patient returned to the emergency department with a similar presentation of severe epigastric abdominal pain and back pain which he related to his typical VOC. This time, there was significantly elevated lipase 8,265 U/L. Right upper quadrant US (RUQUS) revealed cholelithiasis but no choledocholithiasis. Treatment for AP included IVF and pain medications. Seven months later, he was admitted for recurrent AP. Lipase was 7,037 U/L and RUQUS showed intraluminal gallbladder polyps but no cholelithiasis (Figure B). After ruling out all the common etiologies of AP including gallstones, ethanol use, hypertriglyceridemia, steroid use, and autoimmunity, the etiology of recurrent episodes of acute pancreatitis was presumably to be secondary to VOC.
Discussion: Vaso-occlusive crises can present as acute sharp abdominal pain from micro-occlusive infarcts of the mesentery and abdominal viscera. The clinical presentation may be indistinguishable from other acute intra-abdominal disease processes, like cholecystitis, splenic sequestration, and appendicitis. Vaso-occlusive-induced pancreatitis is not common but is possibly underreported as the diagnosis can be challenging and difficult to differentiate from usual pain crises. Our case illustrates the need to include vaso-occlusive-induced pancreatitis on the list of differential diagnoses when treating patients with SCD and abdominal pain.
Figure: Figure A: Abdominal computed tomography (CT) scan with intravenous contrast demonstrated edematous enlargement of the pancreas, peripancreatic fat stranding, and free fluid; Figure B: Right upper quadrant US demonstrating multiple intraluminal gallbladder echogenic lesions suggestive of polyps (blue arrows).
Disclosures:
Gabriela Mendez indicated no relevant financial relationships.
Laura Fernandez indicated no relevant financial relationships.
Marwah Farooqui indicated no relevant financial relationships.
John Pueringer indicated no relevant financial relationships.
Abdullah Memon indicated no relevant financial relationships.
Gabriela Mendez, MD, Laura Fernandez, MD, Marwah Farooqui, DO, John Pueringer, DO, Abdullah Memon, MD. P1898 - Acute Pancreatitis in the Setting of Vaso-Occlusive Sickle Cell Crisis: A Rare Etiology, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
