Monday Poster Session
Category: Biliary/Pancreas
P1900 - A Case of Pancreatic Adenocarcinoma Masquerading as Cholangiocarcinoma Due to Pancreatic Atrophy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tulika Saggar, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Tulika Saggar, MD1, Atul Sinha, MD1, James R. Pellegrini, MD2, Ana P. Rivera, MD3, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1
1Nassau University Medical Center, East Meadow, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, Amityville, NY
Introduction: Pancreatic cancer is one the deadliest cancers in the United States, with a 5-year survival rate of about 13% and about 1% when diagnosed at stage IV. Unfortunately, pancreatic cancer is not detected in its early stages due to its location causing a lack of symptoms. Diagnostic imaging is often used in the workup of pancreatic cancer to detect lesions. We present a case of an elderly male diagnosed with pancreatic adenocarcinoma whose mass lesion was not detected on cross-sectional imaging due to pancreatic atrophy.
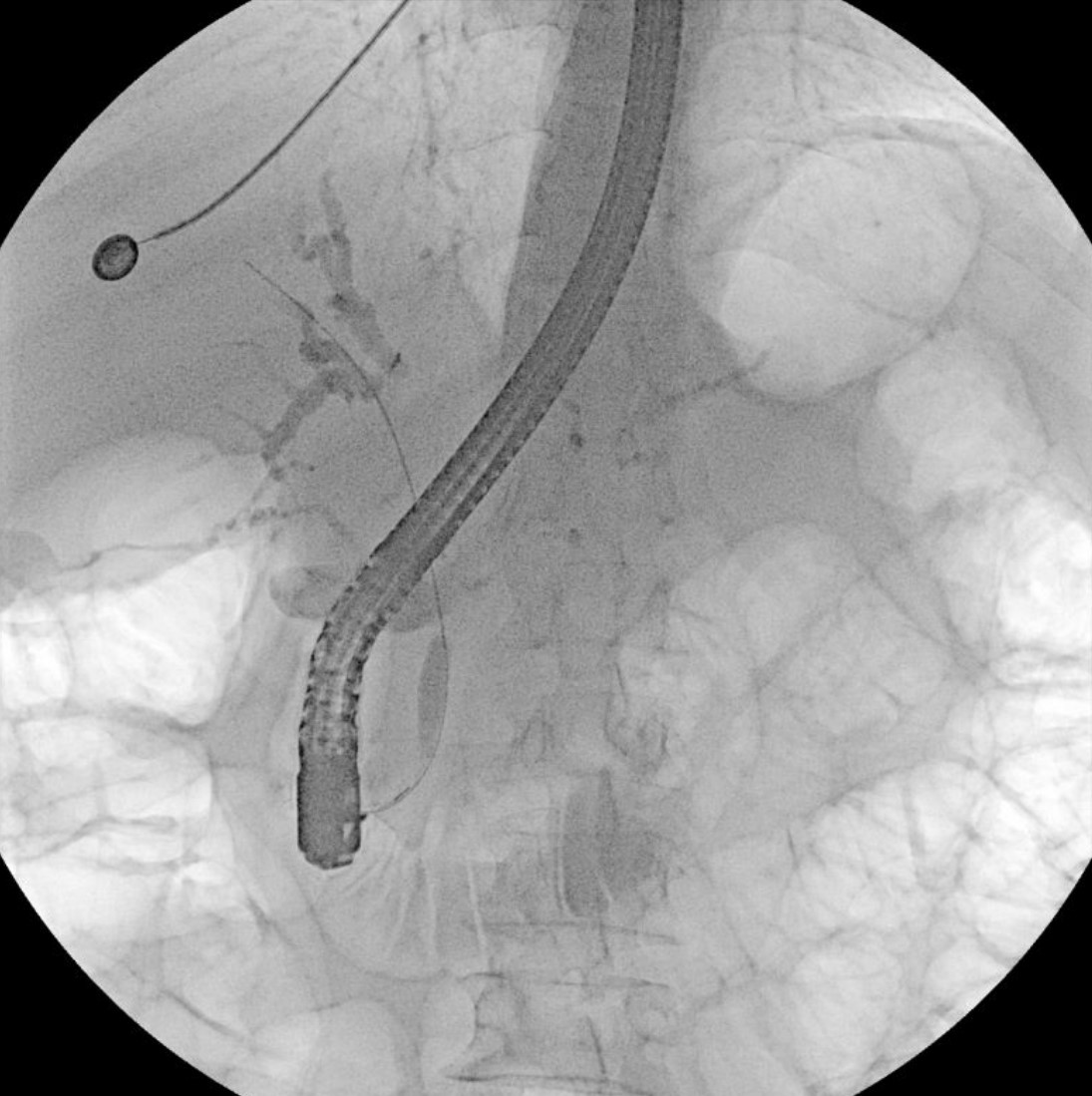
Case Description/Methods: A 79 year-old male with a history of diabetes, hypertension and dementia presented with one month of abdominal pain. As per the patient's daughter, the patient has had yellowing of the skin and lost 20 lbs over the last month. Initial labs showed ALT 103, AST 125, ALP 609, and bilirubin 29.1. CT showed significant dilatation of the intra and extrahepatic biliary ducts and pancreatic duct along with atrophy of the pancreatic body and tail. MRI/MRCP showed focal stenosis of common bile duct, obstruction of pancreatic duct at level of pancreatic neck, and diffuse atrophy of the pancreatic body and tail. No definite focal lesions were identified. ERCP was performed with placement of biliary stent for decompression. Cytology of bushings were positive for clusters of large marked atypical cells with prominent nucleoli suggestive of adenocarcinoma. Patient underwent open pancreaticoduodenectomy for suspected cholangiocarcinoma. Biopsy results from the common bile duct were normal, however, biopsies from the head of the pancreas showed invasive pancreatic duct adenocarcinoma. Patient is following with oncology for adjuvant chemotherapy.
Discussion: This case highlights the difficulty of diagnosing pancreatic mass lesions in the setting of pancreatic atrophy. The underlying lesion resulted in compression of the bile duct, leading to the false diagnosis of cholangiocarcinoma. Fortunately, the correct diagnosis was made with surgical biopsies and the patient was initiated on proper treatment. Physicians treating patients with any pancreatic pathology must have heightened suspicion when their patient has pancreatic atrophy. Without increased awareness, diagnosis may be missed and patient outcomes will be worse, particularly when treating pancreatic adenocarcinoma.
Disclosures:
Tulika Saggar, MD1, Atul Sinha, MD1, James R. Pellegrini, MD2, Ana P. Rivera, MD3, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1. P1900 - A Case of Pancreatic Adenocarcinoma Masquerading as Cholangiocarcinoma Due to Pancreatic Atrophy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nassau University Medical Center, East Meadow, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, Amityville, NY
Introduction: Pancreatic cancer is one the deadliest cancers in the United States, with a 5-year survival rate of about 13% and about 1% when diagnosed at stage IV. Unfortunately, pancreatic cancer is not detected in its early stages due to its location causing a lack of symptoms. Diagnostic imaging is often used in the workup of pancreatic cancer to detect lesions. We present a case of an elderly male diagnosed with pancreatic adenocarcinoma whose mass lesion was not detected on cross-sectional imaging due to pancreatic atrophy.
Case Description/Methods: A 79 year-old male with a history of diabetes, hypertension and dementia presented with one month of abdominal pain. As per the patient's daughter, the patient has had yellowing of the skin and lost 20 lbs over the last month. Initial labs showed ALT 103, AST 125, ALP 609, and bilirubin 29.1. CT showed significant dilatation of the intra and extrahepatic biliary ducts and pancreatic duct along with atrophy of the pancreatic body and tail. MRI/MRCP showed focal stenosis of common bile duct, obstruction of pancreatic duct at level of pancreatic neck, and diffuse atrophy of the pancreatic body and tail. No definite focal lesions were identified. ERCP was performed with placement of biliary stent for decompression. Cytology of bushings were positive for clusters of large marked atypical cells with prominent nucleoli suggestive of adenocarcinoma. Patient underwent open pancreaticoduodenectomy for suspected cholangiocarcinoma. Biopsy results from the common bile duct were normal, however, biopsies from the head of the pancreas showed invasive pancreatic duct adenocarcinoma. Patient is following with oncology for adjuvant chemotherapy.
Discussion: This case highlights the difficulty of diagnosing pancreatic mass lesions in the setting of pancreatic atrophy. The underlying lesion resulted in compression of the bile duct, leading to the false diagnosis of cholangiocarcinoma. Fortunately, the correct diagnosis was made with surgical biopsies and the patient was initiated on proper treatment. Physicians treating patients with any pancreatic pathology must have heightened suspicion when their patient has pancreatic atrophy. Without increased awareness, diagnosis may be missed and patient outcomes will be worse, particularly when treating pancreatic adenocarcinoma.
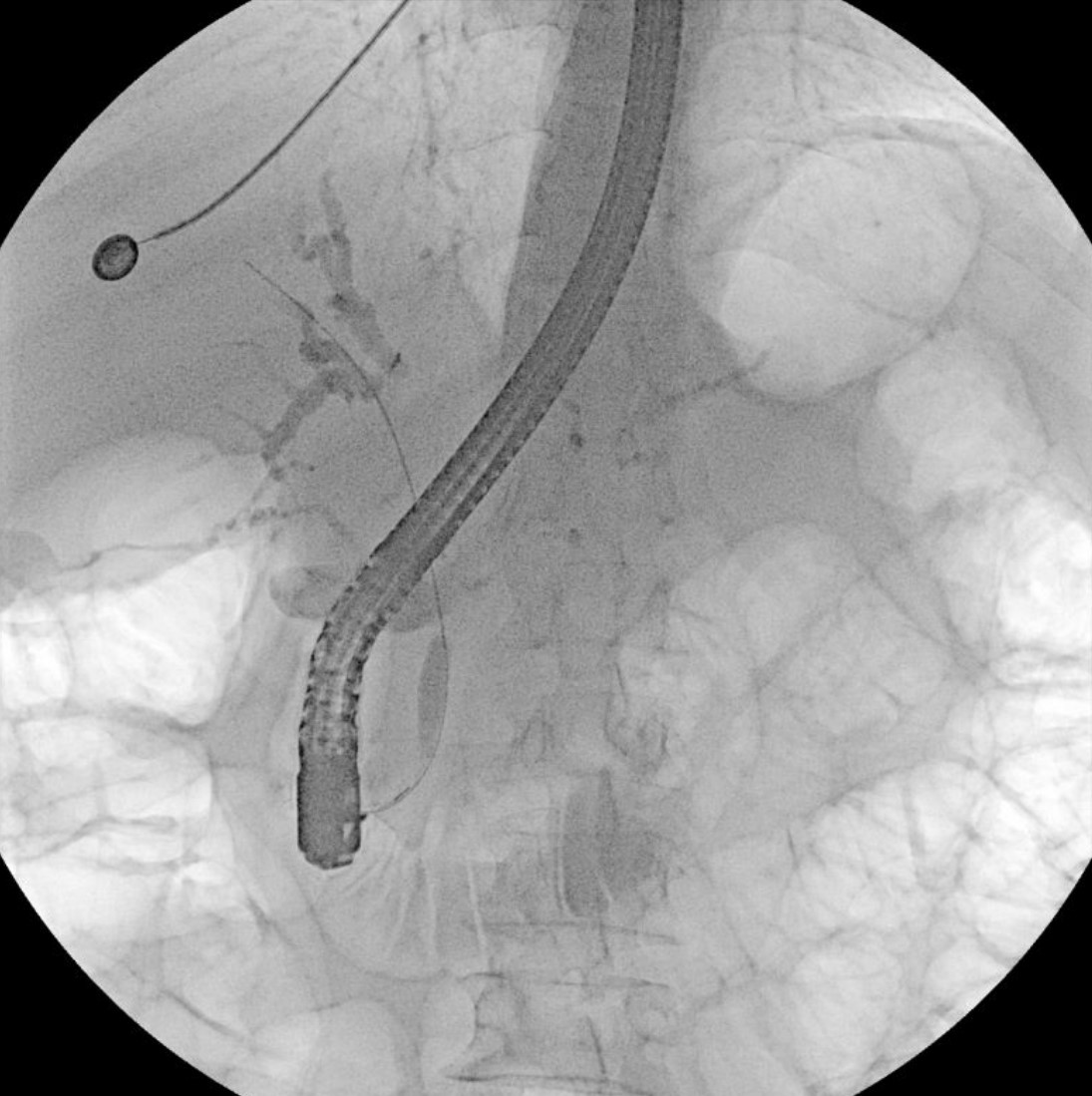
Figure: Focal stenosis of distal common bile duct on endoscopic retrograde cholangiopancreatography
Disclosures:
Tulika Saggar indicated no relevant financial relationships.
Atul Sinha indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Ana Rivera indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Tulika Saggar, MD1, Atul Sinha, MD1, James R. Pellegrini, MD2, Ana P. Rivera, MD3, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1. P1900 - A Case of Pancreatic Adenocarcinoma Masquerading as Cholangiocarcinoma Due to Pancreatic Atrophy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
