Monday Poster Session
Category: Biliary/Pancreas
P1901 - Hemobilia Masquerading as Cholestatic Liver Injury Post Liver Biopsy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Salman Ahmed, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Salman Ahmed, DO, Rachel Patel, DO, Henry Lam, DO, Adam Peyton, MD, Travis Magdaleno, DO
Lehigh Valley Health Network, Allentown, PA
Introduction: Hemobilia is a rare cause of GI bleed. It most commonly arises due to iatrogenic injury resulting in hepatobiliary injury. Here we highlight a rare case of hemobilia causing obstructive jaundice arising after transjugular liver biopsy performed for suspected autoimmune hepatitis.
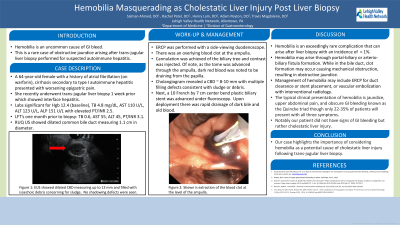
Case Description/Methods: A 64-year-old female with past medical history of atrial fibrillation on warfarin and type I autoimmune hepatitis (AIH) cirrhosis presented to the ER with progressive epigastric pain for several days that worsened with food intake. Pain was partially relieved with NSAIDs. Of note, she recently underwent transjugular liver biopsy 1-week prior which showed an underlying cirrhosis with pathology consistent with interface hepatitis which confirmed suspicion of AIH. Labs on arrival were most significant for abnormal liver function tests: TB 4.8 mg/dL, AST 110 U/L, ALT 123 U/L, ALP 151 U/L with elevated PT/INR 2.5. Initially, the clinical picture was consistent with untreated autoimmune hepatitis. The patient was scheduled for an EGD for variceal screening and to evaluate for peptic ulcer disease given NSAID use. However, RUQ US showed dilated common bile duct measuring 1.1 cm in diameter. Subsequent endoscopic evaluation was performed with an EUS which confirmed a significantly dilated common bile duct measuring up to 13 mm filled with hyperechoic debris suggestive of blood clots. An ERCP was then performed confirming EUS findings. The blood clots were cleared from the duct followed by placement of a plastic biliary stent to maintain patency. Patient was eventually started on prednisone and azathioprine for underlying AIH. Ultimately, she was diagnosed with obstructive jaundice secondary to hemobilia after recent transjugular liver biopsy.
Discussion: Hemobilia is an exceedingly rare complication that can arise after liver biopsy. It has an incidence of < 1% and can occur immediately or in a delayed fashion. Interesting, our patient did not have any signs of overt GI bleed but rather features of cholestatic liver injury. Hemobilia may arise through portal-biliary or arterio-biliary fistula formation. While in the bile duct, clot formation may occur causing mechanical obstruction, resulting in obstructive jaundice. Management of hemobilia may include ERCP for duct clearance or stent placement, or vascular embolization with interventional radiology. Our case highlights the importance of considering hemobilia as a potential complication following transjugular liver biopsy.
Disclosures:
Salman Ahmed, DO, Rachel Patel, DO, Henry Lam, DO, Adam Peyton, MD, Travis Magdaleno, DO. P1901 - Hemobilia Masquerading as Cholestatic Liver Injury Post Liver Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lehigh Valley Health Network, Allentown, PA
Introduction: Hemobilia is a rare cause of GI bleed. It most commonly arises due to iatrogenic injury resulting in hepatobiliary injury. Here we highlight a rare case of hemobilia causing obstructive jaundice arising after transjugular liver biopsy performed for suspected autoimmune hepatitis.
Case Description/Methods: A 64-year-old female with past medical history of atrial fibrillation on warfarin and type I autoimmune hepatitis (AIH) cirrhosis presented to the ER with progressive epigastric pain for several days that worsened with food intake. Pain was partially relieved with NSAIDs. Of note, she recently underwent transjugular liver biopsy 1-week prior which showed an underlying cirrhosis with pathology consistent with interface hepatitis which confirmed suspicion of AIH. Labs on arrival were most significant for abnormal liver function tests: TB 4.8 mg/dL, AST 110 U/L, ALT 123 U/L, ALP 151 U/L with elevated PT/INR 2.5. Initially, the clinical picture was consistent with untreated autoimmune hepatitis. The patient was scheduled for an EGD for variceal screening and to evaluate for peptic ulcer disease given NSAID use. However, RUQ US showed dilated common bile duct measuring 1.1 cm in diameter. Subsequent endoscopic evaluation was performed with an EUS which confirmed a significantly dilated common bile duct measuring up to 13 mm filled with hyperechoic debris suggestive of blood clots. An ERCP was then performed confirming EUS findings. The blood clots were cleared from the duct followed by placement of a plastic biliary stent to maintain patency. Patient was eventually started on prednisone and azathioprine for underlying AIH. Ultimately, she was diagnosed with obstructive jaundice secondary to hemobilia after recent transjugular liver biopsy.
Discussion: Hemobilia is an exceedingly rare complication that can arise after liver biopsy. It has an incidence of < 1% and can occur immediately or in a delayed fashion. Interesting, our patient did not have any signs of overt GI bleed but rather features of cholestatic liver injury. Hemobilia may arise through portal-biliary or arterio-biliary fistula formation. While in the bile duct, clot formation may occur causing mechanical obstruction, resulting in obstructive jaundice. Management of hemobilia may include ERCP for duct clearance or stent placement, or vascular embolization with interventional radiology. Our case highlights the importance of considering hemobilia as a potential complication following transjugular liver biopsy.
Disclosures:
Salman Ahmed indicated no relevant financial relationships.
Rachel Patel indicated no relevant financial relationships.
Henry Lam indicated no relevant financial relationships.
Adam Peyton indicated no relevant financial relationships.
Travis Magdaleno indicated no relevant financial relationships.
Salman Ahmed, DO, Rachel Patel, DO, Henry Lam, DO, Adam Peyton, MD, Travis Magdaleno, DO. P1901 - Hemobilia Masquerading as Cholestatic Liver Injury Post Liver Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

