Monday Poster Session
Category: Biliary/Pancreas
P1905 - The Elusive In-Patient Management of Hypertriglyceridemia Induced Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Simur Khurana, BS
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Simur Khurana, BS1, Shannon Blee, MS1, Maya Samuel, BS1, Mason Jones, MD1, Thomas Cheketts, DO1, Michael Shaw, DO2
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Hypertriglyceridemia (HTG) is responsible for up to 10% of acute pancreatitis cases. The mechanism of inflammation in hypertriglyceridemic pancreatitis (HTGP) is thought to be secondary to ischemia caused by an increase in plasma viscosity. Though the presentation and hospital course of HTGP is similar to other causes of pancreatitis, the elevation of triglycerides is associated with a greater risk of complications and requires urgent intervention. Treatment options for HTGP may include starting a weight-based insulin drip and plasmapheresis. Because hospitals typically only have a protocol for glucose-based insulin drip, implementing a weight-based drip often requires providers to create their own weight-based protocol, as outlined in this case.
Case Description/Methods: A 69 yo M. with a history of HLD, T2DM, CAD and HFrEF (35%) presented with centralized abdominal pain, nausea, and vomiting. CT revealed peripancreatic fat stranding. Lipase on admission was 3825 and his triglycerides (TG) 4926. Calculated Apache-II score was > 8 indicating severe disease and he was admitted to the medical floor. Treatment for HTPG was initiated with IV fluids. An insulin regimen of 0.1mg/kg/hr was ordered with dextrose titrated to maintain a blood glucose of > 150. The following morning TG levels decreased to 3583. Due to hospital policy restricting weight-based insulin drips he was transitioned to a glucose-based titration protocol and automatically transferred to the ICU. Plasmapheresis was initiated, reducing TG levels to 483. He was then transitioned from IV to subcutaneous insulin with daily fenofibrate 48 mg and atorvastatin 40 mg. On day 4, his TG levels increased to 603, and his fenofibrate was increased to 145 mg and atorvastatin to 80 mg. TG levels subsequently stabilized.
Discussion: HTGP is symptomatically indistinguishable from other cases of pancreatitis, yet the management is unique. Plasmapheresis is an important treatment for HTGP but takes time to set up and could delay care if solely relied upon. In this case, treatment was interrupted due to a lack of policy for a weight-based insulin regimen. A protocol titrating weight-based insulin and dextrose with the goal to maintain a constant glucose level could have prevented this patient's interruption in care. The current ACG guidelines do not specify a preferred treatment approach for HTGP. A standardization of management and protocol should be considered to prevent complications in these high risk patients.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Simur Khurana, BS1, Shannon Blee, MS1, Maya Samuel, BS1, Mason Jones, MD1, Thomas Cheketts, DO1, Michael Shaw, DO2. P1905 - The Elusive In-Patient Management of Hypertriglyceridemia Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Hypertriglyceridemia (HTG) is responsible for up to 10% of acute pancreatitis cases. The mechanism of inflammation in hypertriglyceridemic pancreatitis (HTGP) is thought to be secondary to ischemia caused by an increase in plasma viscosity. Though the presentation and hospital course of HTGP is similar to other causes of pancreatitis, the elevation of triglycerides is associated with a greater risk of complications and requires urgent intervention. Treatment options for HTGP may include starting a weight-based insulin drip and plasmapheresis. Because hospitals typically only have a protocol for glucose-based insulin drip, implementing a weight-based drip often requires providers to create their own weight-based protocol, as outlined in this case.
Case Description/Methods: A 69 yo M. with a history of HLD, T2DM, CAD and HFrEF (35%) presented with centralized abdominal pain, nausea, and vomiting. CT revealed peripancreatic fat stranding. Lipase on admission was 3825 and his triglycerides (TG) 4926. Calculated Apache-II score was > 8 indicating severe disease and he was admitted to the medical floor. Treatment for HTPG was initiated with IV fluids. An insulin regimen of 0.1mg/kg/hr was ordered with dextrose titrated to maintain a blood glucose of > 150. The following morning TG levels decreased to 3583. Due to hospital policy restricting weight-based insulin drips he was transitioned to a glucose-based titration protocol and automatically transferred to the ICU. Plasmapheresis was initiated, reducing TG levels to 483. He was then transitioned from IV to subcutaneous insulin with daily fenofibrate 48 mg and atorvastatin 40 mg. On day 4, his TG levels increased to 603, and his fenofibrate was increased to 145 mg and atorvastatin to 80 mg. TG levels subsequently stabilized.
Discussion: HTGP is symptomatically indistinguishable from other cases of pancreatitis, yet the management is unique. Plasmapheresis is an important treatment for HTGP but takes time to set up and could delay care if solely relied upon. In this case, treatment was interrupted due to a lack of policy for a weight-based insulin regimen. A protocol titrating weight-based insulin and dextrose with the goal to maintain a constant glucose level could have prevented this patient's interruption in care. The current ACG guidelines do not specify a preferred treatment approach for HTGP. A standardization of management and protocol should be considered to prevent complications in these high risk patients.

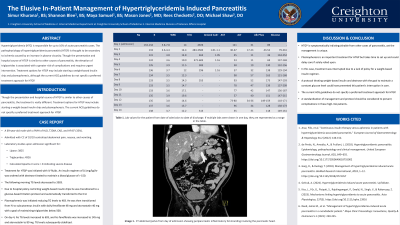
Figure: Image 1. CT abdomen/pelvis from day of admission showing peripancreatic inflammatory fat stranding involving the pancreatic head.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Simur Khurana indicated no relevant financial relationships.
Shannon Blee indicated no relevant financial relationships.
Maya Samuel indicated no relevant financial relationships.
Mason Jones indicated no relevant financial relationships.
Thomas Cheketts indicated no relevant financial relationships.
Michael Shaw indicated no relevant financial relationships.
Simur Khurana, BS1, Shannon Blee, MS1, Maya Samuel, BS1, Mason Jones, MD1, Thomas Cheketts, DO1, Michael Shaw, DO2. P1905 - The Elusive In-Patient Management of Hypertriglyceridemia Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
