Monday Poster Session
Category: Biliary/Pancreas
P1907 - Acute Cholangitis and Endoscopic Interventions: The Need to Tailor Our Treatment Approach.
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- QA
Qusai Almasad, MD
Roger Williams Medical Center
Providence, RI
Presenting Author(s)
Qusai Almasad, MD, Aryanna Sousa, MD, MPH, Paola Pena, MD, Guljana Saeed, MD, Cristian Hiraldo-Infante, MD
Roger Williams Medical Center, Providence, RI
Introduction: Acute cholangitis is a life-threatening condition. Drainage under endoscopic retrograde cholangiopancreatography (ERCP) is the treatment of choice. However, suboptimal clinical outcomes necessitate a tailored treatment approach. We present a case where the patient underwent multiple endoscopic interventions.
Case Description/Methods: A 78-year-old female was referred for evaluation of progressive jaundice. Her abdominal CT revealed intra and extrahepatic ductal dilatation with a filling defect in the distal common bile duct, raising concern for a suspected underlying lesion causing an obstruction. Her hospital course involved diagnosing acute cholangitis, where she was treated with antibiotics and subsequently underwent an endoscopic ultrasound. Sonography revealed an intramural lesion in the ampulla with dilation of the common bile duct (12 mm). She failed to respond to initial therapy, developed hypotension, required pressor support, and was transitioned to the Intensive Care Unit. Her diagnosis worsened to severe cholangitis. She subsequently underwent an ERCP with stent placement, with plans for a repeat ERCP with sphincterotomy in 6 weeks. Unfortunately, she further deteriorated clinically. A repeat ERCP was performed within 6 days, along with the removal of the previously placed stent. Her main bile duct was noted to be dilated with multiple stones, indicating choledocholithiasis. A complete removal with biliary sphincterotomy was performed. Despite these measures, her clinical course worsened and the mainstay of her management was redirected towards hospice care.
Discussion: Acute cholangitis can present with varying severity. This case highlights the importance of timely endoscopic interventions as a reliable treatment option with decreasing morbidity and mortality rates. It is imperative to adopt a tailored approach for successfully navigating individual cases. Our approach should rely on identifying crucial prognostic factors and comorbid conditions. Despite improved management, mortality in cases of acute cholangitis remains approximately 5%. No guidelines favor or reject repeating ERCP procedures within close intervals. There remains a notable gap in knowledge with little evidence suggesting the advantage of this approach, thus prompting a reevaluation of its clinical utility based on individual cases. This case illustrates the need to weigh the potential implications of repeating invasive procedures on a patient's clinical course and assess the likelihood of tangible benefits.

Disclosures:
Qusai Almasad, MD, Aryanna Sousa, MD, MPH, Paola Pena, MD, Guljana Saeed, MD, Cristian Hiraldo-Infante, MD. P1907 - Acute Cholangitis and Endoscopic Interventions: The Need to Tailor Our Treatment Approach., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Roger Williams Medical Center, Providence, RI
Introduction: Acute cholangitis is a life-threatening condition. Drainage under endoscopic retrograde cholangiopancreatography (ERCP) is the treatment of choice. However, suboptimal clinical outcomes necessitate a tailored treatment approach. We present a case where the patient underwent multiple endoscopic interventions.
Case Description/Methods: A 78-year-old female was referred for evaluation of progressive jaundice. Her abdominal CT revealed intra and extrahepatic ductal dilatation with a filling defect in the distal common bile duct, raising concern for a suspected underlying lesion causing an obstruction. Her hospital course involved diagnosing acute cholangitis, where she was treated with antibiotics and subsequently underwent an endoscopic ultrasound. Sonography revealed an intramural lesion in the ampulla with dilation of the common bile duct (12 mm). She failed to respond to initial therapy, developed hypotension, required pressor support, and was transitioned to the Intensive Care Unit. Her diagnosis worsened to severe cholangitis. She subsequently underwent an ERCP with stent placement, with plans for a repeat ERCP with sphincterotomy in 6 weeks. Unfortunately, she further deteriorated clinically. A repeat ERCP was performed within 6 days, along with the removal of the previously placed stent. Her main bile duct was noted to be dilated with multiple stones, indicating choledocholithiasis. A complete removal with biliary sphincterotomy was performed. Despite these measures, her clinical course worsened and the mainstay of her management was redirected towards hospice care.
Discussion: Acute cholangitis can present with varying severity. This case highlights the importance of timely endoscopic interventions as a reliable treatment option with decreasing morbidity and mortality rates. It is imperative to adopt a tailored approach for successfully navigating individual cases. Our approach should rely on identifying crucial prognostic factors and comorbid conditions. Despite improved management, mortality in cases of acute cholangitis remains approximately 5%. No guidelines favor or reject repeating ERCP procedures within close intervals. There remains a notable gap in knowledge with little evidence suggesting the advantage of this approach, thus prompting a reevaluation of its clinical utility based on individual cases. This case illustrates the need to weigh the potential implications of repeating invasive procedures on a patient's clinical course and assess the likelihood of tangible benefits.

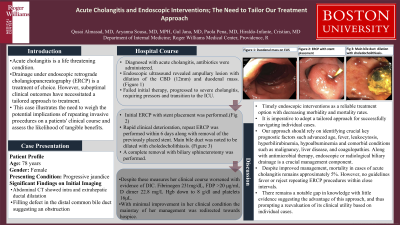
Figure: Figure 1: Duodenal mass on EUS
Figure 2: ERCP with stent placement
Figure 3: Removal of previously placed stent. Main bile duct dilation with choledocholithiasis.
Figure 2: ERCP with stent placement
Figure 3: Removal of previously placed stent. Main bile duct dilation with choledocholithiasis.
Disclosures:
Qusai Almasad indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Paola Pena indicated no relevant financial relationships.
Guljana Saeed indicated no relevant financial relationships.
Cristian Hiraldo-Infante indicated no relevant financial relationships.
Qusai Almasad, MD, Aryanna Sousa, MD, MPH, Paola Pena, MD, Guljana Saeed, MD, Cristian Hiraldo-Infante, MD. P1907 - Acute Cholangitis and Endoscopic Interventions: The Need to Tailor Our Treatment Approach., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
