Monday Poster Session
Category: Colon
P1935 - First-Line Treatment of Fecal Microbiota Transplantation for Immune-Mediated Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- YW
Yinghong Wang, MD, PhD
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Yinghong Wang, MD, PhD1, Krishnavathana Varatharajalu, MD2, Malek Shatila, MD2, Carolina Colli Cruz, MD3, Anusha Thomas, MD2, Herbert DuPont, MD4
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4The University of Texas School of Public Health, Houston, TX
Introduction: The management of moderate to severe IMC requires immunosuppression. Long-term immunosuppression increases the risk for infections and steroid side-effects. Fecal microbiota transplantation (FMT) is increasingly used for the treatment of refractory IMC. Front-line FMT treatment may potentially alleviate IMC symptoms while reducing unnecessary exposure to steroids and their complications. In this study, we present a case series of 15 patients who received front-line FMT for IMC as part of a clinical trial.
Methods: This study reports preliminary data from a prospective clinical trial (NCT0403861) exploring the efficacy and safety of FMT as a first-line treatment for IMC. To be included, patients had to 1) have symptoms of IMC CTCAE grade ≥ 2 within 45 days of FMT and 2) not have received any immunosuppressive treatment for IMC or any other indication around the time of FMT.
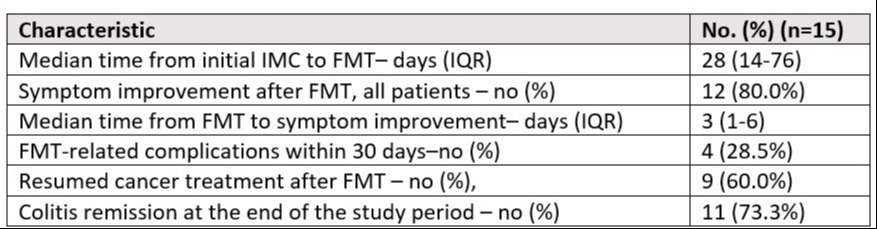
Results: Fifteen patients were enrolled thus far. Patients received front-line FMT in a median of 28 days from IMC onset. 12 (80%) patients had symptom improvement in a median of 3 days (IQR: 1-6 days) after FMT. The only FMT-related adverse events reported were fatigue, transient fever, abdominal cramping and bloating in seven patients (46.6%) within the first week (Table 1). Most patients (12, 80%) stopped immunotherapy due to IMC, but nine patients (60%) were able to resume cancer treatment after FMT, with six (40%) resuming immune checkpoint inhibitors (ICI). None of the patients that resumed ICI had recurrence of their colitis requiring immunosuppression. Eleven patients (73.3%) had colitis remission by the end of the study period, with one additional patient showing signs of symptom improvement but passing away before his outcome could be assessed. Only three patients (20%) required immunosuppression for persistent colitis after FMT failure.
Discussion: This study is the first to evaluate the safety and efficacy of front-line FMT for the treatment of IMC and has demonstrated that FMT can be an effective and safe first-line treatment for IMC that can quickly provide symptom relief in a majority of patients while avoiding the use of steroids. Our results also suggest that front-line FMT can be delivered in a timely manner and can allow for the successful resumption of immunotherapy in this population that typically responds well to immunotherapy.
Disclosures:
Yinghong Wang, MD, PhD1,Krishnavathana Varatharajalu, MD2, Malek Shatila, MD2, Carolina Colli Cruz, MD3, Anusha Thomas, MD2, Herbert DuPont, MD4. P1935 - First-Line Treatment of Fecal Microbiota Transplantation for Immune-Mediated Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Yinghong Wang, MD, PhD1, Krishnavathana Varatharajalu, MD2, Malek Shatila, MD2, Carolina Colli Cruz, MD3, Anusha Thomas, MD2, Herbert DuPont, MD4
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4The University of Texas School of Public Health, Houston, TX
Introduction: The management of moderate to severe IMC requires immunosuppression. Long-term immunosuppression increases the risk for infections and steroid side-effects. Fecal microbiota transplantation (FMT) is increasingly used for the treatment of refractory IMC. Front-line FMT treatment may potentially alleviate IMC symptoms while reducing unnecessary exposure to steroids and their complications. In this study, we present a case series of 15 patients who received front-line FMT for IMC as part of a clinical trial.
Methods: This study reports preliminary data from a prospective clinical trial (NCT0403861) exploring the efficacy and safety of FMT as a first-line treatment for IMC. To be included, patients had to 1) have symptoms of IMC CTCAE grade ≥ 2 within 45 days of FMT and 2) not have received any immunosuppressive treatment for IMC or any other indication around the time of FMT.
Results: Fifteen patients were enrolled thus far. Patients received front-line FMT in a median of 28 days from IMC onset. 12 (80%) patients had symptom improvement in a median of 3 days (IQR: 1-6 days) after FMT. The only FMT-related adverse events reported were fatigue, transient fever, abdominal cramping and bloating in seven patients (46.6%) within the first week (Table 1). Most patients (12, 80%) stopped immunotherapy due to IMC, but nine patients (60%) were able to resume cancer treatment after FMT, with six (40%) resuming immune checkpoint inhibitors (ICI). None of the patients that resumed ICI had recurrence of their colitis requiring immunosuppression. Eleven patients (73.3%) had colitis remission by the end of the study period, with one additional patient showing signs of symptom improvement but passing away before his outcome could be assessed. Only three patients (20%) required immunosuppression for persistent colitis after FMT failure.
Discussion: This study is the first to evaluate the safety and efficacy of front-line FMT for the treatment of IMC and has demonstrated that FMT can be an effective and safe first-line treatment for IMC that can quickly provide symptom relief in a majority of patients while avoiding the use of steroids. Our results also suggest that front-line FMT can be delivered in a timely manner and can allow for the successful resumption of immunotherapy in this population that typically responds well to immunotherapy.
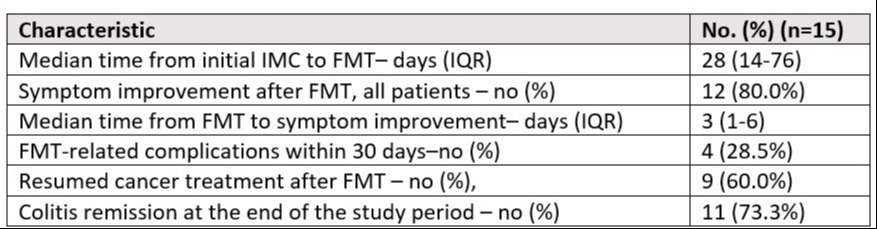
Figure: Table
Disclosures:
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Malek Shatila indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Anusha Thomas indicated no relevant financial relationships.
Herbert DuPont indicated no relevant financial relationships.
Yinghong Wang, MD, PhD1,Krishnavathana Varatharajalu, MD2, Malek Shatila, MD2, Carolina Colli Cruz, MD3, Anusha Thomas, MD2, Herbert DuPont, MD4. P1935 - First-Line Treatment of Fecal Microbiota Transplantation for Immune-Mediated Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

