Monday Poster Session
Category: Colon
P1958 - Outcomes of Endoscopic Submucosal Dissection for Large Colorectal Neoplasms: An International, Multicenter Perspective
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Marina Kim, DO
Assistant Professor of Medicine
Saint Louis University
St. Louis, MO
Presenting Author(s)
Award: Presidential Poster Award
Marina Kim, DO1, Darshan Parekh, MBBS2, Galen Leung, MD3, Yohei Minato, MD4, Yoshiaki Kimoto, MD5, Amit Daphale, MBBS6, Harsh Bapaye, MBBS7, Arun Arora Pagadapelli, MBBS8, Monica Gaidhane, MD9, Michel Kahaleh, MD10, Amol Bapaye, MBBS8, Ken Ohata, MD, PhD4
1Saint Louis University, St. Louis, MO; 2Mumbai Institute of Gastroenterology, Mumbai, Maharashtra, India; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4NTT Medical Center, Shinagawa City, Tokyo, Japan; 5NTT Medical Center, Shinagawa, Tokyo, Japan; 6Shivanand Desai Center for Digestive Disorders, Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India; 7Byramjee Jeejeebhoy Medical College, Pune, Maharashtra, India; 8Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India; 9Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ; 10Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ
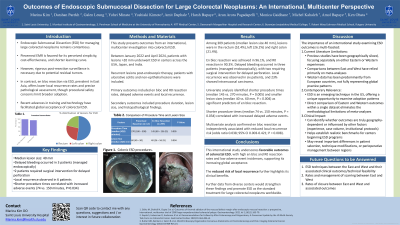
Introduction: dissection (ESD) for managing large colorectal neoplasms remains contentious. Piecemeal EMR is favored for its perceived simplicity, cost-effectiveness, and shorter learning curve. However, rigorous post-resection surveillance is necessary due to potential residual tumors. In contrast, en bloc resection via ESD, prevalent in East Asia, offers lower local recurrence rates and precise pathological assessment, though procedural safety concerns limit broader adoption. Recent advances in training and technology have facilitated global acceptance of colorectal ESD.
Methods: This study presents outcomes from an international, multicenter investigation into colorectal ESD. Between January 2022 and April 2024, patients with lesions >20 mm underwent ESD in centers across the USA, Japan, and India. Recurrent lesions post-endoscopic therapy, patients with ulcerative colitis and non-epithelial lesions were included. Primary outcomes included en bloc and R0 resection rates, delayed adverse events and local recurrence. Secondary outcomes included procedure duration, lesion size, and histopathological findings.
Results: Among 309 patients (median lesion size 40 mm), lesions were in the rectum (52.4%), left (26.2%) and right colon (21.4%). En bloc resection was achieved in 96.1%, and R0 resection in 90.3%. Delayed bleeding occurred in three patients (managed endoscopically), with two requiring surgical intervention for delayed perforation. Local recurrence was observed in six patients, and 23% showed intramucosal carcinoma.
Univariate analysis identified shorter procedure times (median 145 vs. 270 minutes, P = 0.005) and smaller lesion sizes (median 40 vs. 60 mm, P = 0.004) as significant predictors of en bloc resection. Shorter procedure times (median 74 vs. 150 minutes, P = 0.034) correlated with increased adverse events. Multivariate analysis confirmed en bloc resection as independently associated with reduced local recurrence risk (odds ratio 0.038; 95% CI 0.003-0.421; P = 0.008).
Discussion: This international study underscores favorable outcomes of colorectal ESD, with high en bloc and R0 resection rates and low adverse event incidences, supporting its increasing global acceptance. The reduced risk of local recurrence further highlights its clinical benefits. Further data from diverse centers would strengthen these findings and promote ESD as the standard treatment for large colorectal neoplasms worldwide.
Disclosures:
Marina Kim, DO1, Darshan Parekh, MBBS2, Galen Leung, MD3, Yohei Minato, MD4, Yoshiaki Kimoto, MD5, Amit Daphale, MBBS6, Harsh Bapaye, MBBS7, Arun Arora Pagadapelli, MBBS8, Monica Gaidhane, MD9, Michel Kahaleh, MD10, Amol Bapaye, MBBS8, Ken Ohata, MD, PhD4. P1958 - Outcomes of Endoscopic Submucosal Dissection for Large Colorectal Neoplasms: An International, Multicenter Perspective, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Marina Kim, DO1, Darshan Parekh, MBBS2, Galen Leung, MD3, Yohei Minato, MD4, Yoshiaki Kimoto, MD5, Amit Daphale, MBBS6, Harsh Bapaye, MBBS7, Arun Arora Pagadapelli, MBBS8, Monica Gaidhane, MD9, Michel Kahaleh, MD10, Amol Bapaye, MBBS8, Ken Ohata, MD, PhD4
1Saint Louis University, St. Louis, MO; 2Mumbai Institute of Gastroenterology, Mumbai, Maharashtra, India; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4NTT Medical Center, Shinagawa City, Tokyo, Japan; 5NTT Medical Center, Shinagawa, Tokyo, Japan; 6Shivanand Desai Center for Digestive Disorders, Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India; 7Byramjee Jeejeebhoy Medical College, Pune, Maharashtra, India; 8Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India; 9Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ; 10Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ
Introduction: dissection (ESD) for managing large colorectal neoplasms remains contentious. Piecemeal EMR is favored for its perceived simplicity, cost-effectiveness, and shorter learning curve. However, rigorous post-resection surveillance is necessary due to potential residual tumors. In contrast, en bloc resection via ESD, prevalent in East Asia, offers lower local recurrence rates and precise pathological assessment, though procedural safety concerns limit broader adoption. Recent advances in training and technology have facilitated global acceptance of colorectal ESD.
Methods: This study presents outcomes from an international, multicenter investigation into colorectal ESD. Between January 2022 and April 2024, patients with lesions >20 mm underwent ESD in centers across the USA, Japan, and India. Recurrent lesions post-endoscopic therapy, patients with ulcerative colitis and non-epithelial lesions were included. Primary outcomes included en bloc and R0 resection rates, delayed adverse events and local recurrence. Secondary outcomes included procedure duration, lesion size, and histopathological findings.
Results: Among 309 patients (median lesion size 40 mm), lesions were in the rectum (52.4%), left (26.2%) and right colon (21.4%). En bloc resection was achieved in 96.1%, and R0 resection in 90.3%. Delayed bleeding occurred in three patients (managed endoscopically), with two requiring surgical intervention for delayed perforation. Local recurrence was observed in six patients, and 23% showed intramucosal carcinoma.
Univariate analysis identified shorter procedure times (median 145 vs. 270 minutes, P = 0.005) and smaller lesion sizes (median 40 vs. 60 mm, P = 0.004) as significant predictors of en bloc resection. Shorter procedure times (median 74 vs. 150 minutes, P = 0.034) correlated with increased adverse events. Multivariate analysis confirmed en bloc resection as independently associated with reduced local recurrence risk (odds ratio 0.038; 95% CI 0.003-0.421; P = 0.008).
Discussion: This international study underscores favorable outcomes of colorectal ESD, with high en bloc and R0 resection rates and low adverse event incidences, supporting its increasing global acceptance. The reduced risk of local recurrence further highlights its clinical benefits. Further data from diverse centers would strengthen these findings and promote ESD as the standard treatment for large colorectal neoplasms worldwide.
Disclosures:
Marina Kim indicated no relevant financial relationships.
Darshan Parekh indicated no relevant financial relationships.
Galen Leung indicated no relevant financial relationships.
Yohei Minato indicated no relevant financial relationships.
Yoshiaki Kimoto indicated no relevant financial relationships.
Amit Daphale indicated no relevant financial relationships.
Harsh Bapaye indicated no relevant financial relationships.
Arun Arora Pagadapelli indicated no relevant financial relationships.
Monica Gaidhane indicated no relevant financial relationships.
Michel Kahaleh indicated no relevant financial relationships.
Amol Bapaye indicated no relevant financial relationships.
Ken Ohata indicated no relevant financial relationships.
Marina Kim, DO1, Darshan Parekh, MBBS2, Galen Leung, MD3, Yohei Minato, MD4, Yoshiaki Kimoto, MD5, Amit Daphale, MBBS6, Harsh Bapaye, MBBS7, Arun Arora Pagadapelli, MBBS8, Monica Gaidhane, MD9, Michel Kahaleh, MD10, Amol Bapaye, MBBS8, Ken Ohata, MD, PhD4. P1958 - Outcomes of Endoscopic Submucosal Dissection for Large Colorectal Neoplasms: An International, Multicenter Perspective, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

