Monday Poster Session
Category: Colon
P1968 - The Bowel Bug Mystery: Clostridium difficile in the Blood - A Rare Misunderstood Phenomenon
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Samee Farooqi, DO
Advocate Christ Medical Center
Oak Lawn, IL
Presenting Author(s)
Samee Farooqi, DO1, Ahmad Mardini, MD1, Ahmed Abuhasna, DO2, Krishna Shah, MD1, Matthew Posen, DO1, Harreth Raddawi, MD1
1Advocate Christ Medical Center, Oak Lawn, IL; 2Advocate Illinois Masonic Medical Center, Oak Lawn, IL
Introduction: Clostridium difficile (C. difficile) is a gram-positive anaerobic bacillus and is a common bacterium known to cause numerous hospital admissions for diarrhea. Isolation of this organism in extracolonic sites has been rare. Reported extracolonic manifestations include bacteremia, soft tissue infections, empyema, splenic and pancreatic abscesses. Most cases of extracolonic C. difficile have been preceded by gastrointestinal disease, such as colitis or anatomical disruption of the colon. Herein, we describe an unusual case of C. difficile bacteremia without preceding gastrointestinal manifestations.
Case Description/Methods: A 57-year-old female with past medical history of seizure disorder presented to the hospital for fevers, confusion, abdominal pain and constipation. The patient was recently hospitalized three weeks prior for an abdominal wall abscess requiring incision and drainage and discharged on antibiotics. On arrival the patient was hypotensive and febrile with labs notable for white blood cell count of 29.5 K/mcL. Computed tomography abdomen pelvis showed a focal soft tissue density with no intra-abdominal extension concerning for residual abdominal wall abscess. Blood cultures were drawn, and the patient was admitted to the intensive care unit for septic shock. She was started on broad spectrum antibiotics with cefepime, vancomycin, and metronidazole. General surgery was consulted, and the patient underwent a bedside incision and drainage. Blood cultures came back positive for polymicrobial organisms including clostridium difficile susceptible to metronidazole. Patient’s clinical symptoms improved with resolution of infection and repeat blood cultures negative. She was discharged to a subacute rehab facility with an extended course of antibiotics.
Discussion: C. difficile bacteremia, although rare, has been slowly increasing in prevalence. A literature review in 2017 found 60 clinically documented cases from 1962 to 2016 with a mortality rate reaching approximately 35% percent. It is unclear whether bacterial translocation or another underlying disease process such as colonic ischemia, intestinal tract disorders or mucosal barrier disruptions facilitate bacterial dissemination. Due to its high mortality, research and knowledge on pathophysiology as well as the clinical signs and symptoms of extracolonic manifestations of this organism will be helpful in advancing patient care and clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Samee Farooqi, DO1, Ahmad Mardini, MD1, Ahmed Abuhasna, DO2, Krishna Shah, MD1, Matthew Posen, DO1, Harreth Raddawi, MD1. P1968 - The Bowel Bug Mystery: <i>Clostridium difficile</i> in the Blood - A Rare Misunderstood Phenomenon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Advocate Christ Medical Center, Oak Lawn, IL; 2Advocate Illinois Masonic Medical Center, Oak Lawn, IL
Introduction: Clostridium difficile (C. difficile) is a gram-positive anaerobic bacillus and is a common bacterium known to cause numerous hospital admissions for diarrhea. Isolation of this organism in extracolonic sites has been rare. Reported extracolonic manifestations include bacteremia, soft tissue infections, empyema, splenic and pancreatic abscesses. Most cases of extracolonic C. difficile have been preceded by gastrointestinal disease, such as colitis or anatomical disruption of the colon. Herein, we describe an unusual case of C. difficile bacteremia without preceding gastrointestinal manifestations.
Case Description/Methods: A 57-year-old female with past medical history of seizure disorder presented to the hospital for fevers, confusion, abdominal pain and constipation. The patient was recently hospitalized three weeks prior for an abdominal wall abscess requiring incision and drainage and discharged on antibiotics. On arrival the patient was hypotensive and febrile with labs notable for white blood cell count of 29.5 K/mcL. Computed tomography abdomen pelvis showed a focal soft tissue density with no intra-abdominal extension concerning for residual abdominal wall abscess. Blood cultures were drawn, and the patient was admitted to the intensive care unit for septic shock. She was started on broad spectrum antibiotics with cefepime, vancomycin, and metronidazole. General surgery was consulted, and the patient underwent a bedside incision and drainage. Blood cultures came back positive for polymicrobial organisms including clostridium difficile susceptible to metronidazole. Patient’s clinical symptoms improved with resolution of infection and repeat blood cultures negative. She was discharged to a subacute rehab facility with an extended course of antibiotics.
Discussion: C. difficile bacteremia, although rare, has been slowly increasing in prevalence. A literature review in 2017 found 60 clinically documented cases from 1962 to 2016 with a mortality rate reaching approximately 35% percent. It is unclear whether bacterial translocation or another underlying disease process such as colonic ischemia, intestinal tract disorders or mucosal barrier disruptions facilitate bacterial dissemination. Due to its high mortality, research and knowledge on pathophysiology as well as the clinical signs and symptoms of extracolonic manifestations of this organism will be helpful in advancing patient care and clinical outcomes.
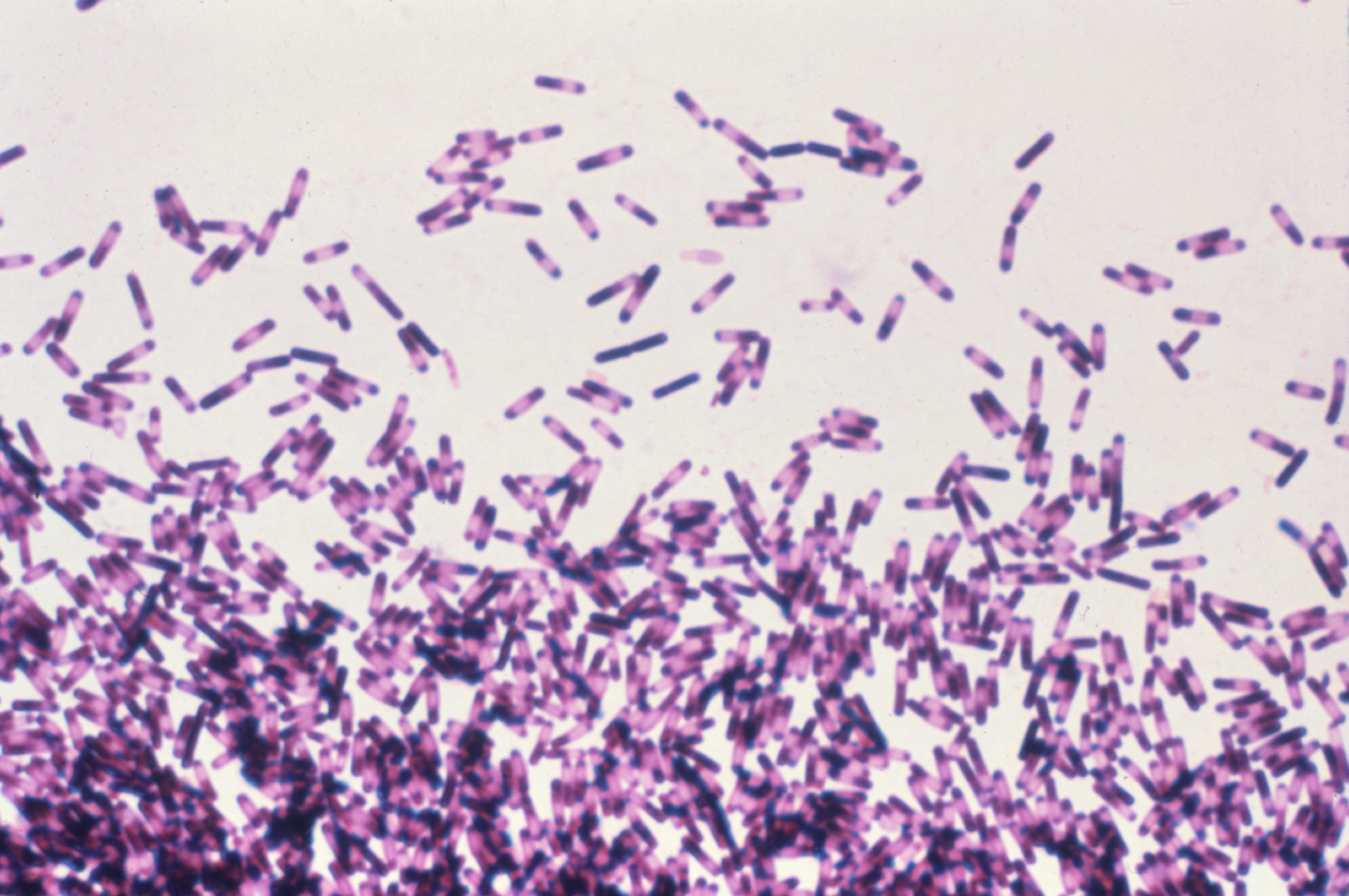
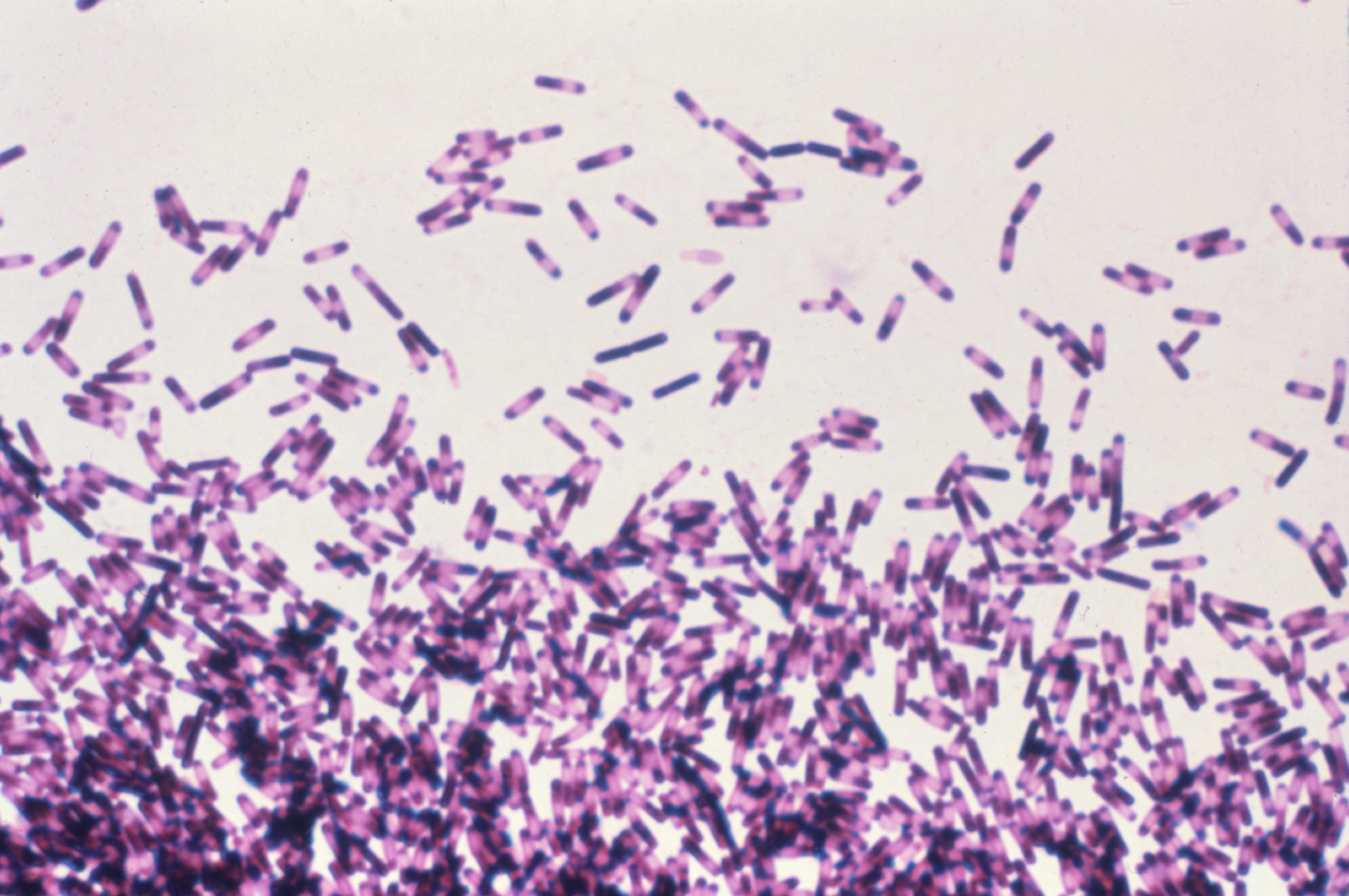
Figure: This photomicrograph reveals the presence of numerous Clostridium difficile bacteria in an impression agar blood smear.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Samee Farooqi indicated no relevant financial relationships.
Ahmad Mardini indicated no relevant financial relationships.
Ahmed Abuhasna indicated no relevant financial relationships.
Krishna Shah indicated no relevant financial relationships.
Matthew Posen indicated no relevant financial relationships.
Harreth Raddawi indicated no relevant financial relationships.
Samee Farooqi, DO1, Ahmad Mardini, MD1, Ahmed Abuhasna, DO2, Krishna Shah, MD1, Matthew Posen, DO1, Harreth Raddawi, MD1. P1968 - The Bowel Bug Mystery: <i>Clostridium difficile</i> in the Blood - A Rare Misunderstood Phenomenon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
