Monday Poster Session
Category: Colon
P1973 - Strongyloidiasis Mimicking Carcinoid Syndrome in an Immunocompetent Host
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shiv Krishnaswamy, MD, MHA
Memorial Healthcare System
Pembroke Pines, FL
Presenting Author(s)
Shiv Krishnaswamy, MD, MHA1, Karine Kasti, MS2, Suset Almuinas de armas, MD1, Andres Reyes-Corcho, MD1
1Memorial Healthcare System, Pembroke Pines, FL; 2FIU College of Medicine, Miami, FL
Introduction: The spectrum of clinical presentation for Strongyloidiasis varies based on the immunological status of the host as well as the chronicity of the parasitic infection. When diagnosing S. stercoralis, stool microscopy and serological testing are the most cited and reliable tests. Stool microscopy for ova and parasites (O&P) remains the gold standard for diagnosing strongyloidiasis. However, this method has been shown to have a baseline low sensitivity for the detection of S. stercoralis due to intermittent excretion of the larvae.
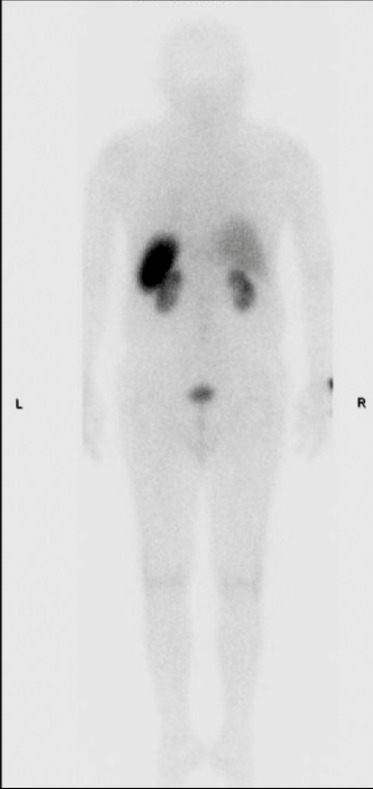
Case Description/Methods: A 72-year-old male was admitted with shortness of breath, chills, and feeling feverish. On physical exam, he had a tender and distended abdomen. CT abdomen/pelvis indicated distal colitis and gastroduodenitis. Complete blood count, erythrocyte sedimentation rate, C-reactive protein, and antinuclear antibody were all within normal limits. Empiric broad spectrum antibiotics were administered but the patient experienced no improvement in his symptoms. A stool O&P, fecal occult blood test, C. difficile panel were unremarkable. The patient then elected to undergo esophagogastroduodenoscopy and colonoscopy; testing for Heliobacter pylori, microscopic colitis, celiac disease, and Whipple’s disease were negative. The workup then shifted towards a neuroendocrine tumor which included urine studies for 5-hydroxyindoleacetic acid (5-HIAA) and an octreotide scan. Both tests for carcinoid syndrome were unrevealing and thus we revisited helminthic infection. Studies for Strongyloides came back positive. The patient was subsequently treated with two doses of oral ivermectin and reported the resolution of his symptoms over the next few days.
Discussion: The diagnosis of S. stercoralis requires a high degree of clinical suspicion due to the lack of validated testing. Eosinophilia is often reported as a diagnostic marker in parasitic infections but is only present when the immune regulatory cells react to the parasite or its products. For direct parasitological detection, a single stool examination has limited sensitivity to diagnose chronic Strongyloides. This particular presentation prompted us to explore the possibility of carcinoid syndrome and a potential neuroendocrine tumor. Strongyloides is known for mimicking other diseases including Crohn’s disease and ulcerative colitis.
Disclosures:
Shiv Krishnaswamy, MD, MHA1, Karine Kasti, MS2, Suset Almuinas de armas, MD1, Andres Reyes-Corcho, MD1. P1973 - Strongyloidiasis Mimicking Carcinoid Syndrome in an Immunocompetent Host, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Memorial Healthcare System, Pembroke Pines, FL; 2FIU College of Medicine, Miami, FL
Introduction: The spectrum of clinical presentation for Strongyloidiasis varies based on the immunological status of the host as well as the chronicity of the parasitic infection. When diagnosing S. stercoralis, stool microscopy and serological testing are the most cited and reliable tests. Stool microscopy for ova and parasites (O&P) remains the gold standard for diagnosing strongyloidiasis. However, this method has been shown to have a baseline low sensitivity for the detection of S. stercoralis due to intermittent excretion of the larvae.
Case Description/Methods: A 72-year-old male was admitted with shortness of breath, chills, and feeling feverish. On physical exam, he had a tender and distended abdomen. CT abdomen/pelvis indicated distal colitis and gastroduodenitis. Complete blood count, erythrocyte sedimentation rate, C-reactive protein, and antinuclear antibody were all within normal limits. Empiric broad spectrum antibiotics were administered but the patient experienced no improvement in his symptoms. A stool O&P, fecal occult blood test, C. difficile panel were unremarkable. The patient then elected to undergo esophagogastroduodenoscopy and colonoscopy; testing for Heliobacter pylori, microscopic colitis, celiac disease, and Whipple’s disease were negative. The workup then shifted towards a neuroendocrine tumor which included urine studies for 5-hydroxyindoleacetic acid (5-HIAA) and an octreotide scan. Both tests for carcinoid syndrome were unrevealing and thus we revisited helminthic infection. Studies for Strongyloides came back positive. The patient was subsequently treated with two doses of oral ivermectin and reported the resolution of his symptoms over the next few days.
Discussion: The diagnosis of S. stercoralis requires a high degree of clinical suspicion due to the lack of validated testing. Eosinophilia is often reported as a diagnostic marker in parasitic infections but is only present when the immune regulatory cells react to the parasite or its products. For direct parasitological detection, a single stool examination has limited sensitivity to diagnose chronic Strongyloides. This particular presentation prompted us to explore the possibility of carcinoid syndrome and a potential neuroendocrine tumor. Strongyloides is known for mimicking other diseases including Crohn’s disease and ulcerative colitis.
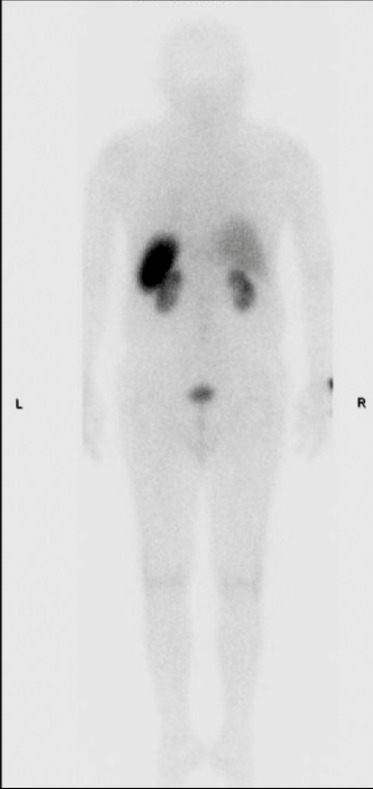
Figure: Octreotide scan demonstrating the absence of somatostatin-positive tumors.
Disclosures:
Shiv Krishnaswamy indicated no relevant financial relationships.
Karine Kasti indicated no relevant financial relationships.
Suset Almuinas de armas indicated no relevant financial relationships.
Andres Reyes-Corcho indicated no relevant financial relationships.
Shiv Krishnaswamy, MD, MHA1, Karine Kasti, MS2, Suset Almuinas de armas, MD1, Andres Reyes-Corcho, MD1. P1973 - Strongyloidiasis Mimicking Carcinoid Syndrome in an Immunocompetent Host, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
