Monday Poster Session
Category: Colon
P1975 - Splenic Abscess Due to Entamoeba Histolytica
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MK
Matthew A. Kalloo, MD
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Matthew A. Kalloo, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Amebiasis, though globally significant, is rare in the United States (US). Even in endemic areas of Asia, Africa, and Central and South America, most infections (80%) are asymptomatic. Nevertheless, amebiasis is responsible for up to 100,000 deaths annually. When symptomatic, Ameba usually presents with dysentery, weight loss, and abdominal pain. Liver abscess is not uncommon. Respiratory, cardiac, and brain infections are rare. We report the exceedingly rare complication of splenic abscess in an immigrant making a circuitous journey to the US.
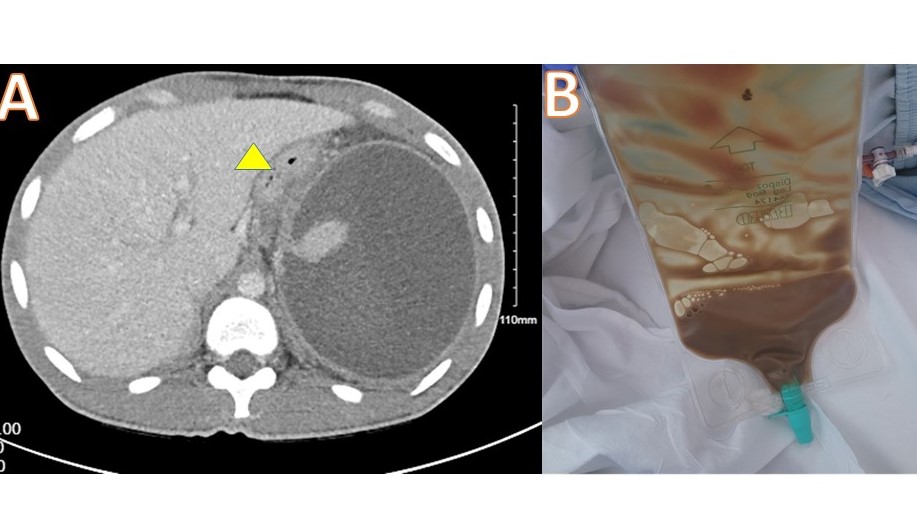
Case Description/Methods: A 23-year-old man from Guinea in West Africa with a past history significant for sickle cell trait, presented to our emergency department for the evaluation of fever. Three weeks before his first ED presentation, he began his migration to the US through the jungles of Central America and crossed the border in Mexico. At his first ED visit, 1 week prior to admission, he complained of fevers and abdominal pain. He was diagnosed with falciparum malaria and prescribed medication that he was unable to obtain. On the day of admission, he presented again to the ED complaining of severe left abdominal pain, and fevers and was noted to have a thrombocytosis (932k/mcL) and a monocytosis (19.1%). Liver panel revealed: AST 44, ALT 66, Alk P 177, Direct bilirubin < 0.2, total bilirubin 0.3 and albumin 3.0. Hemoglobin electrophoresis showed 39.6% HbS. Abdominal CT revealed a large splenic abscess, 13 x 14 cm which drained 1 liter of rust-brown fluid (Figure). The fluid gram stain revealed no white cells or organisms but eventually grew Fusobacterium. Serology was positive for Entameba histolytica. He was given 17 days of Piperacillin/Tazobactam and Metronidazole. Along with albendazole and 3 days of an antimalarial. The drain was removed and he was discharged on 2 weeks of oral metronidazole and amoxicillin/clavulanic acid.
Discussion: Splenic abscesses are exceedingly rare and usually pyogenic. The fluid from this abscess more resembled the ‘anchovy sauce’ description of amebic abscesses. It was also notably devoid of white cells and bacteria, which is more consistent with ameba. We suspect that this patient’s trek through the jungle contracting malaria may have led to the development of a splenic infarct that became secondarily infected with ameba and then bacteria. Sickle trait with over 35% HbS can develop splenic infarcts. A thorough travel history and investigation for multiple organisms is key when evaluating foreign nationals.
Disclosures:
Matthew A. Kalloo, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG. P1975 - Splenic Abscess Due to Entamoeba Histolytica, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Amebiasis, though globally significant, is rare in the United States (US). Even in endemic areas of Asia, Africa, and Central and South America, most infections (80%) are asymptomatic. Nevertheless, amebiasis is responsible for up to 100,000 deaths annually. When symptomatic, Ameba usually presents with dysentery, weight loss, and abdominal pain. Liver abscess is not uncommon. Respiratory, cardiac, and brain infections are rare. We report the exceedingly rare complication of splenic abscess in an immigrant making a circuitous journey to the US.
Case Description/Methods: A 23-year-old man from Guinea in West Africa with a past history significant for sickle cell trait, presented to our emergency department for the evaluation of fever. Three weeks before his first ED presentation, he began his migration to the US through the jungles of Central America and crossed the border in Mexico. At his first ED visit, 1 week prior to admission, he complained of fevers and abdominal pain. He was diagnosed with falciparum malaria and prescribed medication that he was unable to obtain. On the day of admission, he presented again to the ED complaining of severe left abdominal pain, and fevers and was noted to have a thrombocytosis (932k/mcL) and a monocytosis (19.1%). Liver panel revealed: AST 44, ALT 66, Alk P 177, Direct bilirubin < 0.2, total bilirubin 0.3 and albumin 3.0. Hemoglobin electrophoresis showed 39.6% HbS. Abdominal CT revealed a large splenic abscess, 13 x 14 cm which drained 1 liter of rust-brown fluid (Figure). The fluid gram stain revealed no white cells or organisms but eventually grew Fusobacterium. Serology was positive for Entameba histolytica. He was given 17 days of Piperacillin/Tazobactam and Metronidazole. Along with albendazole and 3 days of an antimalarial. The drain was removed and he was discharged on 2 weeks of oral metronidazole and amoxicillin/clavulanic acid.
Discussion: Splenic abscesses are exceedingly rare and usually pyogenic. The fluid from this abscess more resembled the ‘anchovy sauce’ description of amebic abscesses. It was also notably devoid of white cells and bacteria, which is more consistent with ameba. We suspect that this patient’s trek through the jungle contracting malaria may have led to the development of a splenic infarct that became secondarily infected with ameba and then bacteria. Sickle trait with over 35% HbS can develop splenic infarcts. A thorough travel history and investigation for multiple organisms is key when evaluating foreign nationals.
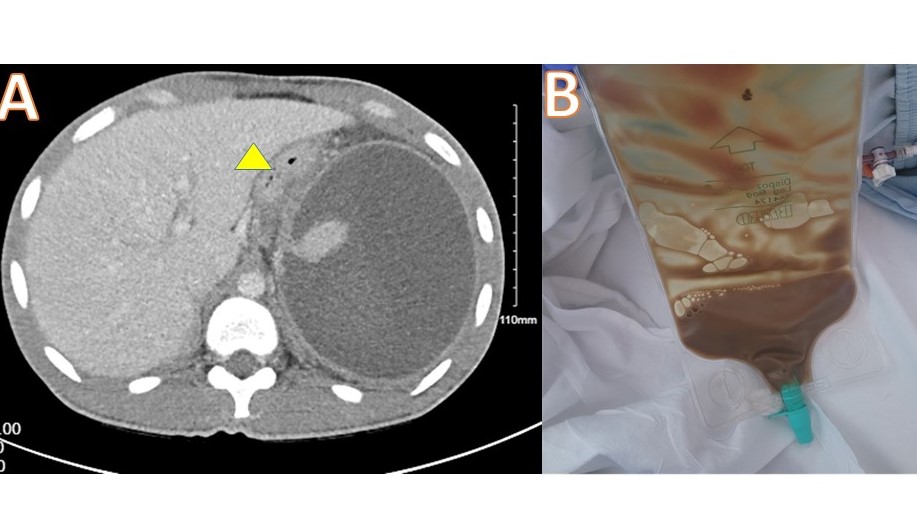
Figure: A: Abdominal CT. Stomach yellow arrowhead. Large round splenic abscess. B: Anchovy sauce aspirate from splenic abscess
Disclosures:
Matthew Kalloo indicated no relevant financial relationships.
Mohamed Osman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Matthew A. Kalloo, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG. P1975 - Splenic Abscess Due to Entamoeba Histolytica, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
