Monday Poster Session
Category: Colon
P2036 - Aggressive Behavior of Immune-Mediated Toxicities Following Immune Checkpoint Inhibitor Therapy Rechallenge
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CC
Carolina Colli Cruz, MD
MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Krishnavathana Varatharajalu, MD1, Carolina Colli Cruz, MD2, Malek Shatila, MD1, Yinghong Wang, MD, PhD3
1The University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune checkpoint inhibitors (ICI) augment immune system activation, enabling it to optimally target and eliminate tumor cells in cancer therapy. Conversely, they may trigger the onset of immune-related adverse events (irAEs), which manifest as toxicities across various organs. Inhibiting cytotoxic T-lymphocyte antigen 4 (CTLA-4) enhances CD28 binding to CD80/86, boosting IL-2 and its receptor expression, strengthening T-cell response. Also, it reduces Treg cell inhibitory effect. The blockage of programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1), reduces peripheral, conversely, self-tolerance.
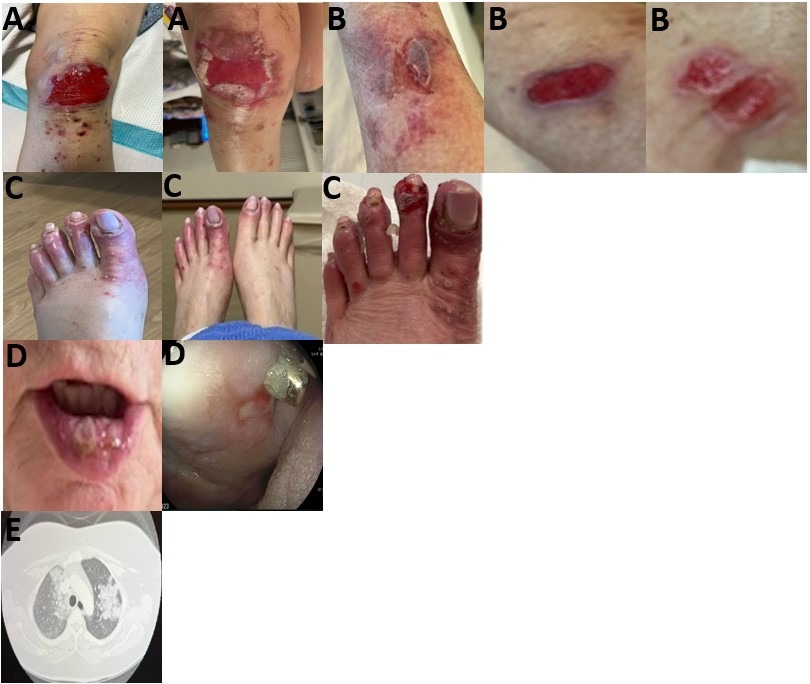
Case Description/Methods: Case: A 78-year-old female with a history of breast cancer, post-segmentectomy, radiation and anastrozole treatment six years ago. Presented with new diagnosis of mesothelioma and was treated with nivolumab (Nivo) and ipilimumab (Ipi) two years ago. Post-first cycle, patient developed immune-mediated diarrhea and colitis (IMDC) that was unresponsive to diphenoxylate-atropine. Colonoscopy and pathology indicated moderate active colitis throughout the colon. Patient failed prednisone and four doses of vedolizumab, eventually achieved complete remission to fecal microbiota transplantation (FMT). A year later, cancer recurrence necessitated Nivo and Ipi resumption. After three doses, her IMDC recurred prompting ICI cessation and steroid treatment. A second FMT led to IMDC resolution and resumption of ICI. However, subsequently she developed a series of irAEs involving multiple organ sites. Initially progressive shortness of breath led to hospitalization, confirming pneumonitis via bronchoscopy and CT scan, for which she was treated with intravenous steroid and a single dose of infliximab with partial response. Then mucositis was diagnosed and treated with mouthwash containing diphenhydramine, lidocaine, nystatin, steroid, and aluminum hydroxide and ganciclovir. Later, patient developed minor excoriations on her skin (legs, toes), which progressed to non-healing shallow ulcers, pathology suggested immune-related skin toxicities. Similarly, back lesions evolved into papules with similar pathology. Evolution raised suspicion for associated vasculitis, unresolved despite steroid use. Figure 1 summarized all the relevant evidence.
Discussion: This case’s novelty lies in development of severe irAEs across multiple organs upon ICI rechallenge post initial single site involvement despite ongoing irAE treatment.
Disclosures:
Krishnavathana Varatharajalu, MD1, Carolina Colli Cruz, MD2, Malek Shatila, MD1, Yinghong Wang, MD, PhD3. P2036 - Aggressive Behavior of Immune-Mediated Toxicities Following Immune Checkpoint Inhibitor Therapy Rechallenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune checkpoint inhibitors (ICI) augment immune system activation, enabling it to optimally target and eliminate tumor cells in cancer therapy. Conversely, they may trigger the onset of immune-related adverse events (irAEs), which manifest as toxicities across various organs. Inhibiting cytotoxic T-lymphocyte antigen 4 (CTLA-4) enhances CD28 binding to CD80/86, boosting IL-2 and its receptor expression, strengthening T-cell response. Also, it reduces Treg cell inhibitory effect. The blockage of programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1), reduces peripheral, conversely, self-tolerance.
Case Description/Methods: Case: A 78-year-old female with a history of breast cancer, post-segmentectomy, radiation and anastrozole treatment six years ago. Presented with new diagnosis of mesothelioma and was treated with nivolumab (Nivo) and ipilimumab (Ipi) two years ago. Post-first cycle, patient developed immune-mediated diarrhea and colitis (IMDC) that was unresponsive to diphenoxylate-atropine. Colonoscopy and pathology indicated moderate active colitis throughout the colon. Patient failed prednisone and four doses of vedolizumab, eventually achieved complete remission to fecal microbiota transplantation (FMT). A year later, cancer recurrence necessitated Nivo and Ipi resumption. After three doses, her IMDC recurred prompting ICI cessation and steroid treatment. A second FMT led to IMDC resolution and resumption of ICI. However, subsequently she developed a series of irAEs involving multiple organ sites. Initially progressive shortness of breath led to hospitalization, confirming pneumonitis via bronchoscopy and CT scan, for which she was treated with intravenous steroid and a single dose of infliximab with partial response. Then mucositis was diagnosed and treated with mouthwash containing diphenhydramine, lidocaine, nystatin, steroid, and aluminum hydroxide and ganciclovir. Later, patient developed minor excoriations on her skin (legs, toes), which progressed to non-healing shallow ulcers, pathology suggested immune-related skin toxicities. Similarly, back lesions evolved into papules with similar pathology. Evolution raised suspicion for associated vasculitis, unresolved despite steroid use. Figure 1 summarized all the relevant evidence.
Discussion: This case’s novelty lies in development of severe irAEs across multiple organs upon ICI rechallenge post initial single site involvement despite ongoing irAE treatment.
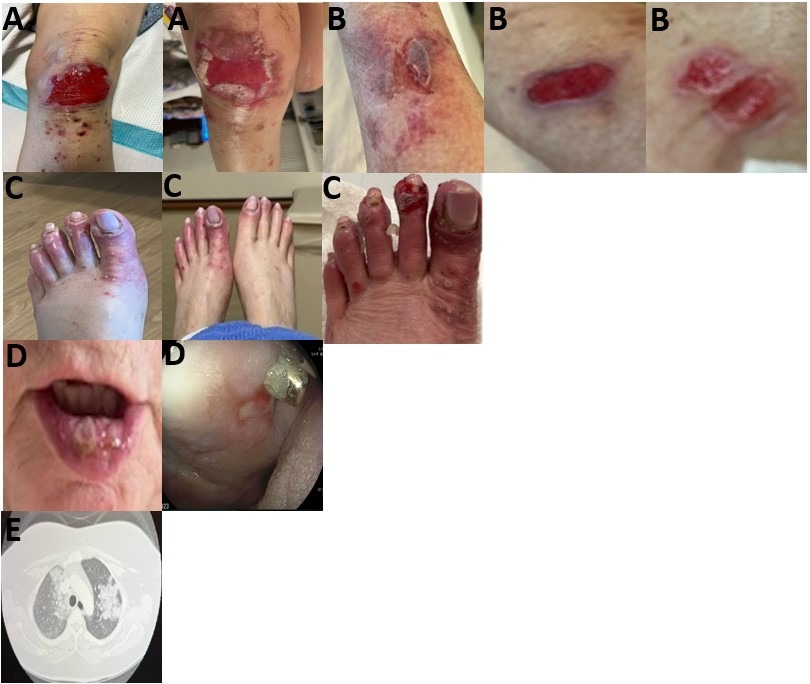
Figure: Title: Multiple irAEs upon ICI rechallenge.
A. Development of open lesions from minor excoriations.
B. Spontaneous eruption of papules and progression with suspicious of vasculitis and/or pyoderma gangrenosum.
C. Skin lesions and slough-off.
D. Mucositis and stomatitis.
E. Pneumonitis on contrast-enhanced CT-Scan.
A. Development of open lesions from minor excoriations.
B. Spontaneous eruption of papules and progression with suspicious of vasculitis and/or pyoderma gangrenosum.
C. Skin lesions and slough-off.
D. Mucositis and stomatitis.
E. Pneumonitis on contrast-enhanced CT-Scan.
Disclosures:
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Malek Shatila indicated no relevant financial relationships.
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Krishnavathana Varatharajalu, MD1, Carolina Colli Cruz, MD2, Malek Shatila, MD1, Yinghong Wang, MD, PhD3. P2036 - Aggressive Behavior of Immune-Mediated Toxicities Following Immune Checkpoint Inhibitor Therapy Rechallenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
