Monday Poster Session
Category: Colon
P2037 - A Case of Colonic Eosinophilia in the Setting of Strongyloidiasis, Ascariasis, and Food Allergy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anveet S. Janwadkar, MD, MBA
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Anveet S. Janwadkar, MD, MBA1, Yucel Aydin, MD1, Catherine T.. Hudson, MD, MPH2
1Tulane School of Medicine, New Orleans, LA; 2LSU, New Orleans, LA
Introduction: Strongyloidiasis and ascariasis are parasitic infections caused by the roundworms Strongyloides stercoralis and Ascaris lumbricoides, respectively. Transmission occurs via contact with contaminated soil, most commonly in tropical and subtropical regions. Infection is often underdiagnosed due to presence of nonspecific symptoms. We present a case of colonic eosinophilia discovered on screening colonoscopy that led to a diagnosis of strongyloidiasis and ascariasis.
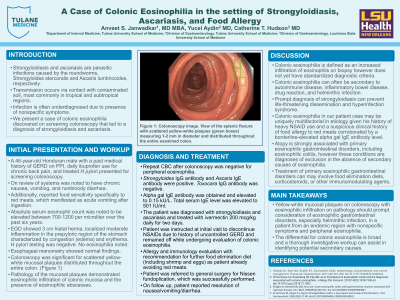
Case Description/Methods: A 46-year-old Honduran male with a past medical history of GERD secondary to 3 cm hiatal hernia, daily NSAID use for chronic pain, treated H pylori, and food sensitivity to red meats presented for screening colonoscopy. Absolute serum eosinophil count was noted to be elevated between 700-1200 per microliter over the past six years. Colonoscopy was significant for scattered yellow-white mucosal plaques measuring 1-2 mm in diameter distributed throughout the entire colon. Biopsy demonstrated eosinophilic infiltration of colonic mucosa and the presence of eosinophilic abscesses. Repeat testing was negative for peripheral eosinophilia. Infectious evaluation was positive for both Strongyloides IgG antibody and Ascaris IgE antibody, but negative for Toxocara IgG antibody. Given previous history of vomiting upon ingestion of red meats (beef and pork), alpha gal IgE antibody was obtained and elevated to 0.15 kU/L. Total serum IgE level was elevated to 501 IU/ml. The patient was diagnosed with strongyloidiasis and ascariasis and treated with ivermectin 200 mcg/kg daily for two days.
Discussion: Colonic eosinophilia can often be secondary to autoimmune disease, inflammatory bowel disease, drug reaction, and helminthic infection. Helminthic infection should be considered in the setting of yellow-white mucosal plaques on colonoscopy in an otherwise asymptomatic patient from an endemic region. Prompt diagnosis of strongyloidiasis can prevent life-threatening dissemination and hyperinfection syndrome. The diagnosis of colonic eosinophilia in our patient case may be uniquely multifactorial in etiology given his history of food sensitivity to red meats with associated elevated alpha gal IgE antibody. Atopy is strongly associated with primary eosinophilic gastrointestinal disorders, including eosinophilic colitis. The persistence of colonic eosinophilia on repeat colonoscopy and improvement of symptoms with food elimination diet may support this diagnosis in the future.
Disclosures:
Anveet S. Janwadkar, MD, MBA1, Yucel Aydin, MD1, Catherine T.. Hudson, MD, MPH2. P2037 - A Case of Colonic Eosinophilia in the Setting of Strongyloidiasis, Ascariasis, and Food Allergy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tulane School of Medicine, New Orleans, LA; 2LSU, New Orleans, LA
Introduction: Strongyloidiasis and ascariasis are parasitic infections caused by the roundworms Strongyloides stercoralis and Ascaris lumbricoides, respectively. Transmission occurs via contact with contaminated soil, most commonly in tropical and subtropical regions. Infection is often underdiagnosed due to presence of nonspecific symptoms. We present a case of colonic eosinophilia discovered on screening colonoscopy that led to a diagnosis of strongyloidiasis and ascariasis.
Case Description/Methods: A 46-year-old Honduran male with a past medical history of GERD secondary to 3 cm hiatal hernia, daily NSAID use for chronic pain, treated H pylori, and food sensitivity to red meats presented for screening colonoscopy. Absolute serum eosinophil count was noted to be elevated between 700-1200 per microliter over the past six years. Colonoscopy was significant for scattered yellow-white mucosal plaques measuring 1-2 mm in diameter distributed throughout the entire colon. Biopsy demonstrated eosinophilic infiltration of colonic mucosa and the presence of eosinophilic abscesses. Repeat testing was negative for peripheral eosinophilia. Infectious evaluation was positive for both Strongyloides IgG antibody and Ascaris IgE antibody, but negative for Toxocara IgG antibody. Given previous history of vomiting upon ingestion of red meats (beef and pork), alpha gal IgE antibody was obtained and elevated to 0.15 kU/L. Total serum IgE level was elevated to 501 IU/ml. The patient was diagnosed with strongyloidiasis and ascariasis and treated with ivermectin 200 mcg/kg daily for two days.
Discussion: Colonic eosinophilia can often be secondary to autoimmune disease, inflammatory bowel disease, drug reaction, and helminthic infection. Helminthic infection should be considered in the setting of yellow-white mucosal plaques on colonoscopy in an otherwise asymptomatic patient from an endemic region. Prompt diagnosis of strongyloidiasis can prevent life-threatening dissemination and hyperinfection syndrome. The diagnosis of colonic eosinophilia in our patient case may be uniquely multifactorial in etiology given his history of food sensitivity to red meats with associated elevated alpha gal IgE antibody. Atopy is strongly associated with primary eosinophilic gastrointestinal disorders, including eosinophilic colitis. The persistence of colonic eosinophilia on repeat colonoscopy and improvement of symptoms with food elimination diet may support this diagnosis in the future.
Disclosures:
Anveet Janwadkar indicated no relevant financial relationships.
Yucel Aydin indicated no relevant financial relationships.
Catherine Hudson indicated no relevant financial relationships.
Anveet S. Janwadkar, MD, MBA1, Yucel Aydin, MD1, Catherine T.. Hudson, MD, MPH2. P2037 - A Case of Colonic Eosinophilia in the Setting of Strongyloidiasis, Ascariasis, and Food Allergy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
