Monday Poster Session
Category: Colon
P2045 - Primary Rectal GIST: A Case Series and Literature Review
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MK
Mehwish Kishore, MD
University of Illinois College of Medicine
Peoria, IL
Presenting Author(s)
Mehwish Kishore, MD1, Jonathan Ragheb, MD2, Matthew Hill, BA1, Srinivas Puli, MD1
1University of Illinois College of Medicine, Peoria, IL; 2Cleveland Clinic Florida, Weston, FL
Introduction: Rectal gastrointestinal stromal tumors (rGISTs) are relatively rare, accounting for about 3–5% of GISTs, and originate from the interstitial cells of Cajal. This single-center retrospective case series will discuss the features and evolution in the management of primary rGIST.
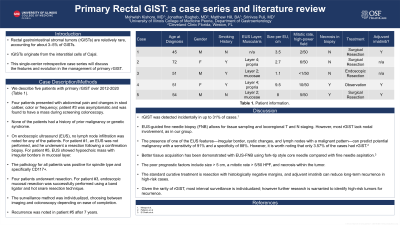
Case Description/Methods: We describe 5 patients with primary rGIST over 2012-2020 (Table 1). Four patients presented with abdominal pain and changes in stool caliber, color or frequency; patient#3 was asymptomatic and was found to have a mass during screening colonoscopy. None of the patients had a history of prior malignancy or genetic syndrome. On endoscopic ultrasound (EUS), no lymph node infiltration was noted for any of the patients. For patient #1, an EUS was not performed, and he underwent a resection following a confirmation biopsy. For patient #5, EUS showed hypoechoic mass with irregular borders in mucosal layer. The pathology for all patients was positive for spindle type and specifically CD117+. Four patients underwent resection. For patient #3, endoscopic mucosal resection was successfully performed using a band ligator and hot snare resection technique. The surveillance method was individualized, choosing between imaging and colonoscopy depending on ease of completion. Recurrence was noted in patient#5 after 7 years.
Discussion: Menge el al. found that rGIST was detected incidentally in up to 31% of cases. EUS-guided fine needle biopsy (FNB) allows for tissue sampling and locoregional T and N staging. However, most rGIST lack nodal involvement, as in our group. Palazzo et al. showed that the presence of one of the EUS features—irregular border, cystic changes, and lymph nodes with a malignant pattern—can predict potential malignancy with a sensitivity of 91% and a specificity of 88%. However, it is worth noting that only 3.57% of the cases had rGIST. El Chafic et al. demonstrated better tissue acquisition with EUS-FNB using fork-tip style core needle compared with fine needle aspiration. The poor prognostic factors include size > 5 cm, a mitotic rate > 5/50 HPF, and necrosis within the tumor. The standard curative treatment is resection with histologically negative margins, and adjuvant imatinib can reduce long-term recurrence in high-risk cases. Given the rarity of rGIST, most interval surveillance is individualized; however further research is warranted to identify high-risk tumors for recurrence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehwish Kishore, MD1, Jonathan Ragheb, MD2, Matthew Hill, BA1, Srinivas Puli, MD1. P2045 - Primary Rectal GIST: A Case Series and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Peoria, IL; 2Cleveland Clinic Florida, Weston, FL
Introduction: Rectal gastrointestinal stromal tumors (rGISTs) are relatively rare, accounting for about 3–5% of GISTs, and originate from the interstitial cells of Cajal. This single-center retrospective case series will discuss the features and evolution in the management of primary rGIST.
Case Description/Methods: We describe 5 patients with primary rGIST over 2012-2020 (Table 1). Four patients presented with abdominal pain and changes in stool caliber, color or frequency; patient#3 was asymptomatic and was found to have a mass during screening colonoscopy. None of the patients had a history of prior malignancy or genetic syndrome. On endoscopic ultrasound (EUS), no lymph node infiltration was noted for any of the patients. For patient #1, an EUS was not performed, and he underwent a resection following a confirmation biopsy. For patient #5, EUS showed hypoechoic mass with irregular borders in mucosal layer. The pathology for all patients was positive for spindle type and specifically CD117+. Four patients underwent resection. For patient #3, endoscopic mucosal resection was successfully performed using a band ligator and hot snare resection technique. The surveillance method was individualized, choosing between imaging and colonoscopy depending on ease of completion. Recurrence was noted in patient#5 after 7 years.
Discussion: Menge el al. found that rGIST was detected incidentally in up to 31% of cases. EUS-guided fine needle biopsy (FNB) allows for tissue sampling and locoregional T and N staging. However, most rGIST lack nodal involvement, as in our group. Palazzo et al. showed that the presence of one of the EUS features—irregular border, cystic changes, and lymph nodes with a malignant pattern—can predict potential malignancy with a sensitivity of 91% and a specificity of 88%. However, it is worth noting that only 3.57% of the cases had rGIST. El Chafic et al. demonstrated better tissue acquisition with EUS-FNB using fork-tip style core needle compared with fine needle aspiration. The poor prognostic factors include size > 5 cm, a mitotic rate > 5/50 HPF, and necrosis within the tumor. The standard curative treatment is resection with histologically negative margins, and adjuvant imatinib can reduce long-term recurrence in high-risk cases. Given the rarity of rGIST, most interval surveillance is individualized; however further research is warranted to identify high-risk tumors for recurrence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehwish Kishore indicated no relevant financial relationships.
Jonathan Ragheb indicated no relevant financial relationships.
Matthew Hill indicated no relevant financial relationships.
Srinivas Puli indicated no relevant financial relationships.
Mehwish Kishore, MD1, Jonathan Ragheb, MD2, Matthew Hill, BA1, Srinivas Puli, MD1. P2045 - Primary Rectal GIST: A Case Series and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

