Monday Poster Session
Category: Colon
P2049 - Unraveling Severe Pseudomembranous Colitis in an Elderly Patient with a Complex Medical History
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ana P. Rivera Arauz, MD
Nassau University Medical Center
Amityville, NY
Presenting Author(s)
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Nausheer Khan, MD3
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Pseudomembranous colitis (PMC) is a severe inflammatory condition of the colon, often caused by Clostridioides difficile infection (CDI). This condition typically follows antibiotic use and is characterized by diarrhea and pseudomembrane formation on the colonic mucosa. PMC is particularly concerning in elderly patients due to their increased susceptibility and the rising incidence of CDI.
Case Description/Methods: An 80-year-old Hispanic female with dementia, type 2 diabetes mellitus (T2DM), hypertension (HTN), hyperlipidemia (HLD), and chronic kidney disease (CKD) stage 4 presented to the emergency department with severe hypoglycemia (serum glucose 29 mg/dL) following routine blood tests. Her family reported frequent watery diarrhea since her recent hospital discharge after treatment for septic shock from a urinary tract infection (UTI).
Examination revealed the patient in a fetal position without acute distress but with a stage 2 sacral ulcer. Laboratory results showed leukocytosis (WBC: 15.5 × 10^9/L), anemia (HGB: 8.2 g/dL), thrombocytosis (PLT: 867 × 10^9/L), and elevated BUN/Cr (69/4.2 mg/dL). A CT scan showed pancolitis, leading to a colonoscopy.
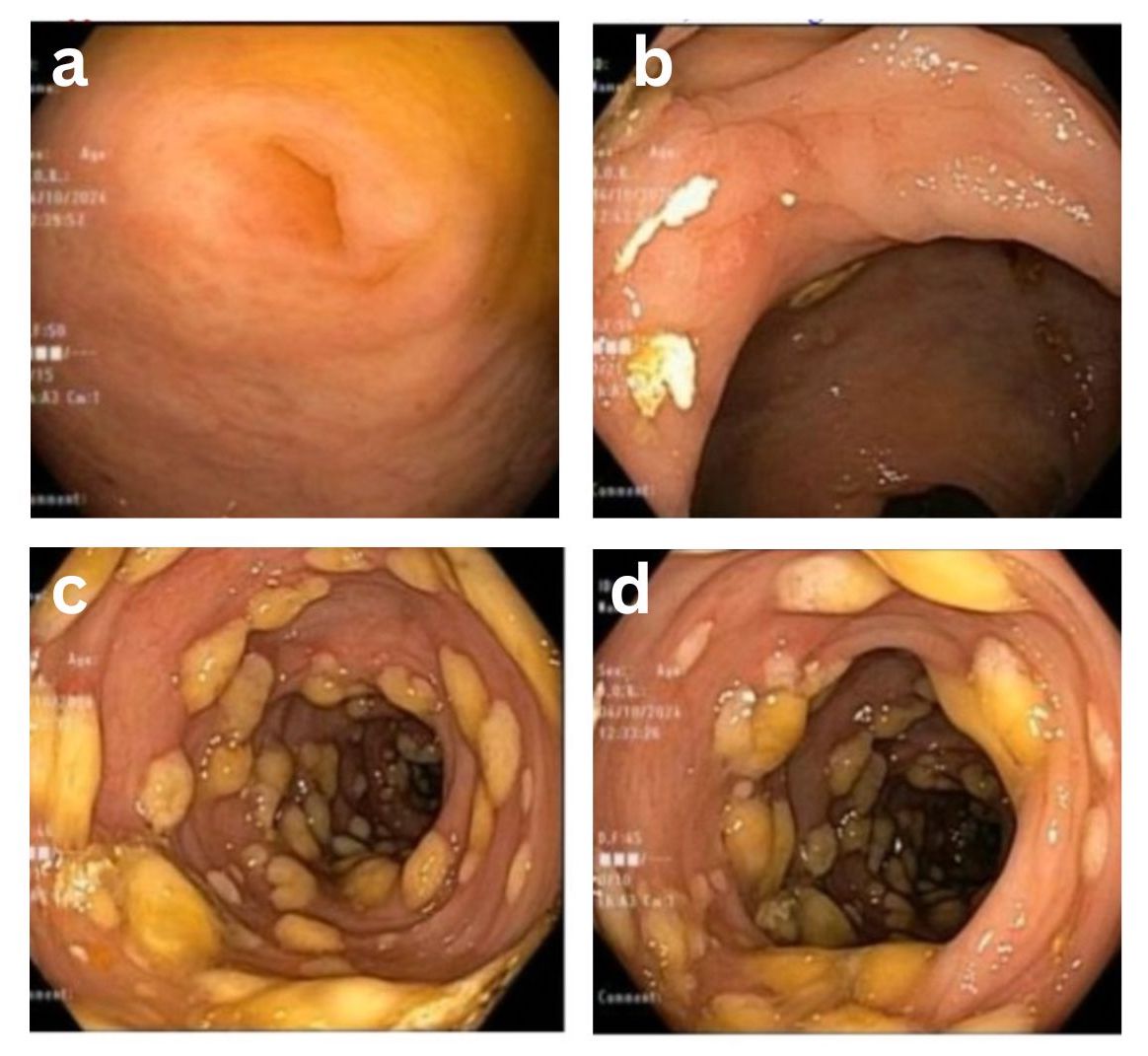
Colonoscopy revealed extensive erythematous mucosa with friable, yellowish pseudomembranes predominantly in the ascending and transverse colon. Additional findings included internal hemorrhoids, an ascending colon ulcer, and a tubular adenoma. Biopsies confirmed severe mucosal necrosis consistent with PMC due to CDI.
She was treated with high-dose oral vancomycin and metronidazole. Despite initial improvement, the patient's condition declined due to severe malnutrition and refusal to comply with treatment, leading to discharge against medical advice.
Discussion: This case highlights the severe implications of PMC in elderly patients with significant comorbidities. The patient's advanced age, CKD, and extensive antibiotic use predisposed her to CDI, with the subsequent colonoscopic findings of pseudomembranes confirming the diagnosis. Her refusal to follow medical and nutritional advice exacerbated her condition, underscoring the complexity of treating elderly patients with cognitive impairments and multiple health issues. Effective management of PMC requires appropriate antimicrobial therapy and supportive care addressing nutritional and psychosocial needs to optimize outcomes. This case illustrates the critical need for tailored treatment strategies in managing elderly patients with severe infections and complex health profiles.
Disclosures:
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Nausheer Khan, MD3. P2049 - Unraveling Severe Pseudomembranous Colitis in an Elderly Patient with a Complex Medical History, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Pseudomembranous colitis (PMC) is a severe inflammatory condition of the colon, often caused by Clostridioides difficile infection (CDI). This condition typically follows antibiotic use and is characterized by diarrhea and pseudomembrane formation on the colonic mucosa. PMC is particularly concerning in elderly patients due to their increased susceptibility and the rising incidence of CDI.
Case Description/Methods: An 80-year-old Hispanic female with dementia, type 2 diabetes mellitus (T2DM), hypertension (HTN), hyperlipidemia (HLD), and chronic kidney disease (CKD) stage 4 presented to the emergency department with severe hypoglycemia (serum glucose 29 mg/dL) following routine blood tests. Her family reported frequent watery diarrhea since her recent hospital discharge after treatment for septic shock from a urinary tract infection (UTI).
Examination revealed the patient in a fetal position without acute distress but with a stage 2 sacral ulcer. Laboratory results showed leukocytosis (WBC: 15.5 × 10^9/L), anemia (HGB: 8.2 g/dL), thrombocytosis (PLT: 867 × 10^9/L), and elevated BUN/Cr (69/4.2 mg/dL). A CT scan showed pancolitis, leading to a colonoscopy.
Colonoscopy revealed extensive erythematous mucosa with friable, yellowish pseudomembranes predominantly in the ascending and transverse colon. Additional findings included internal hemorrhoids, an ascending colon ulcer, and a tubular adenoma. Biopsies confirmed severe mucosal necrosis consistent with PMC due to CDI.
She was treated with high-dose oral vancomycin and metronidazole. Despite initial improvement, the patient's condition declined due to severe malnutrition and refusal to comply with treatment, leading to discharge against medical advice.
Discussion: This case highlights the severe implications of PMC in elderly patients with significant comorbidities. The patient's advanced age, CKD, and extensive antibiotic use predisposed her to CDI, with the subsequent colonoscopic findings of pseudomembranes confirming the diagnosis. Her refusal to follow medical and nutritional advice exacerbated her condition, underscoring the complexity of treating elderly patients with cognitive impairments and multiple health issues. Effective management of PMC requires appropriate antimicrobial therapy and supportive care addressing nutritional and psychosocial needs to optimize outcomes. This case illustrates the critical need for tailored treatment strategies in managing elderly patients with severe infections and complex health profiles.
Figure: Image 1. a: Appendiceal orifice. b. Ascending colon ulcer. c and d: Pan-Pseudomembranous colitis suggestive of C. Diff Colitis.
Disclosures:
Ana Rivera indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Tulika Saggar indicated no relevant financial relationships.
Atul Sinha indicated no relevant financial relationships.
Sandra Gomez indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Nausheer Khan, MD3. P2049 - Unraveling Severe Pseudomembranous Colitis in an Elderly Patient with a Complex Medical History, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
