Monday Poster Session
Category: Colon
P2052 - An Unusual Cause of Hematochezia: Gastrointestinal Amyloidosis Manifesting as Venous Blebs and Submucosal Hematomas
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Namrata Paladugu, BS, MD
University of Mississippi Medical Center
Fort Mill, SC
Presenting Author(s)
Namrata Paladugu, BS, MD, Hamid Ullah, MBBS, Satyapal Chahar, MD, Shou-jiang Tang, MD, Joydeep Chakraborty, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Amyloidosis involves extracellular deposition of precursor misfolded protein fibrils. Light chain immune globulin is the most common protein involved in primary amyloidosis (AL). AL is associated with multiple myeloma (MM) in 15% of patients, and 8% of patients may have gastrointestinal (GI) involvement, most commonly involving the small intestine. Here we present a rare case in which a patient with MM presented with a lower GI bleed and was found to have GI amyloidosis involving the colon.
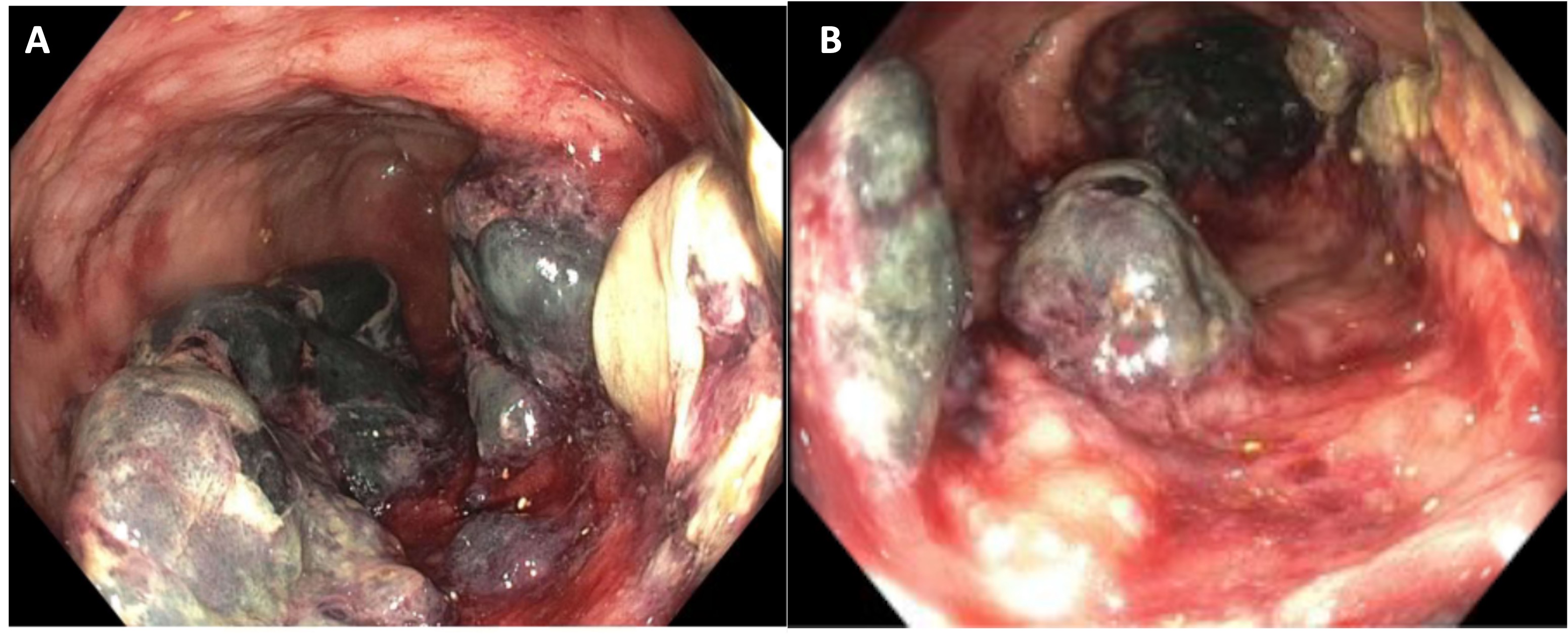
Case Description/Methods: A 61-year-old female with a history of pulmonary embolism on enoxaparin, pulmonary hypertension on riociguat, and MM on cyclophosphamide-bortezomib-dexamethasone therapy presented with hematochezia accompanied by abdominal pain and cramping. She was hemodynamically stable and had no abdominal tenderness or distention. On admission, hemoglobin was 8.3 g/dL and platelet count was 102 TH/cmm. Riociguat and enoxaparin were held, and patient was started on pantoprazole. Colonoscopy showed multiple areas in the sigmoid and descending colon which appeared as venous blebs or submucosal hematomas with surrounding erythema, erosions, and ulcerations which were biopsied. Pathology reported mucosal ulceration with necroinflammatory infiltrate and no suggestion of ischemic colitis. Computed tomography of abdomen and pelvis did not reveal signs of ischemic bowel. As the diagnosis remained unclear, flexible sigmoidoscopy with biopsy was pursued and we requested our pathologist to assess for amyloidosis due to patient’s history of MM. Histopathology revealed amorphous eosinophilic material around submucosal blood vessels staining positive with Congo red and crystal violet, consistent with GI amyloidosis. Immunohistochemistry showed a few CD138 positive cells and in situ hybridization (ISH) revealed few cells positive for kappa and lambda light chains, not consistent with plasma cell neoplasm. Her course was complicated by worsening renal function and hypercapnia requiring intubation.
Discussion: Management of GI amyloidosis relies on treatment of the underlying MM and suppression of amyloid precursor. Early detection and initiation of therapy is key to survival, and prognosis depends on extent of organ involvement. Endoscopic findings are nonspecific and could include colonic ulcers, blebs and submucosal hematomas. GI amyloidosis should be on the differential in patients with MM presenting with a lower GI bleed to ensure early diagnosis and avoid delaying management.
Disclosures:
Namrata Paladugu, BS, MD, Hamid Ullah, MBBS, Satyapal Chahar, MD, Shou-jiang Tang, MD, Joydeep Chakraborty, MD. P2052 - An Unusual Cause of Hematochezia: Gastrointestinal Amyloidosis Manifesting as Venous Blebs and Submucosal Hematomas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Amyloidosis involves extracellular deposition of precursor misfolded protein fibrils. Light chain immune globulin is the most common protein involved in primary amyloidosis (AL). AL is associated with multiple myeloma (MM) in 15% of patients, and 8% of patients may have gastrointestinal (GI) involvement, most commonly involving the small intestine. Here we present a rare case in which a patient with MM presented with a lower GI bleed and was found to have GI amyloidosis involving the colon.
Case Description/Methods: A 61-year-old female with a history of pulmonary embolism on enoxaparin, pulmonary hypertension on riociguat, and MM on cyclophosphamide-bortezomib-dexamethasone therapy presented with hematochezia accompanied by abdominal pain and cramping. She was hemodynamically stable and had no abdominal tenderness or distention. On admission, hemoglobin was 8.3 g/dL and platelet count was 102 TH/cmm. Riociguat and enoxaparin were held, and patient was started on pantoprazole. Colonoscopy showed multiple areas in the sigmoid and descending colon which appeared as venous blebs or submucosal hematomas with surrounding erythema, erosions, and ulcerations which were biopsied. Pathology reported mucosal ulceration with necroinflammatory infiltrate and no suggestion of ischemic colitis. Computed tomography of abdomen and pelvis did not reveal signs of ischemic bowel. As the diagnosis remained unclear, flexible sigmoidoscopy with biopsy was pursued and we requested our pathologist to assess for amyloidosis due to patient’s history of MM. Histopathology revealed amorphous eosinophilic material around submucosal blood vessels staining positive with Congo red and crystal violet, consistent with GI amyloidosis. Immunohistochemistry showed a few CD138 positive cells and in situ hybridization (ISH) revealed few cells positive for kappa and lambda light chains, not consistent with plasma cell neoplasm. Her course was complicated by worsening renal function and hypercapnia requiring intubation.
Discussion: Management of GI amyloidosis relies on treatment of the underlying MM and suppression of amyloid precursor. Early detection and initiation of therapy is key to survival, and prognosis depends on extent of organ involvement. Endoscopic findings are nonspecific and could include colonic ulcers, blebs and submucosal hematomas. GI amyloidosis should be on the differential in patients with MM presenting with a lower GI bleed to ensure early diagnosis and avoid delaying management.
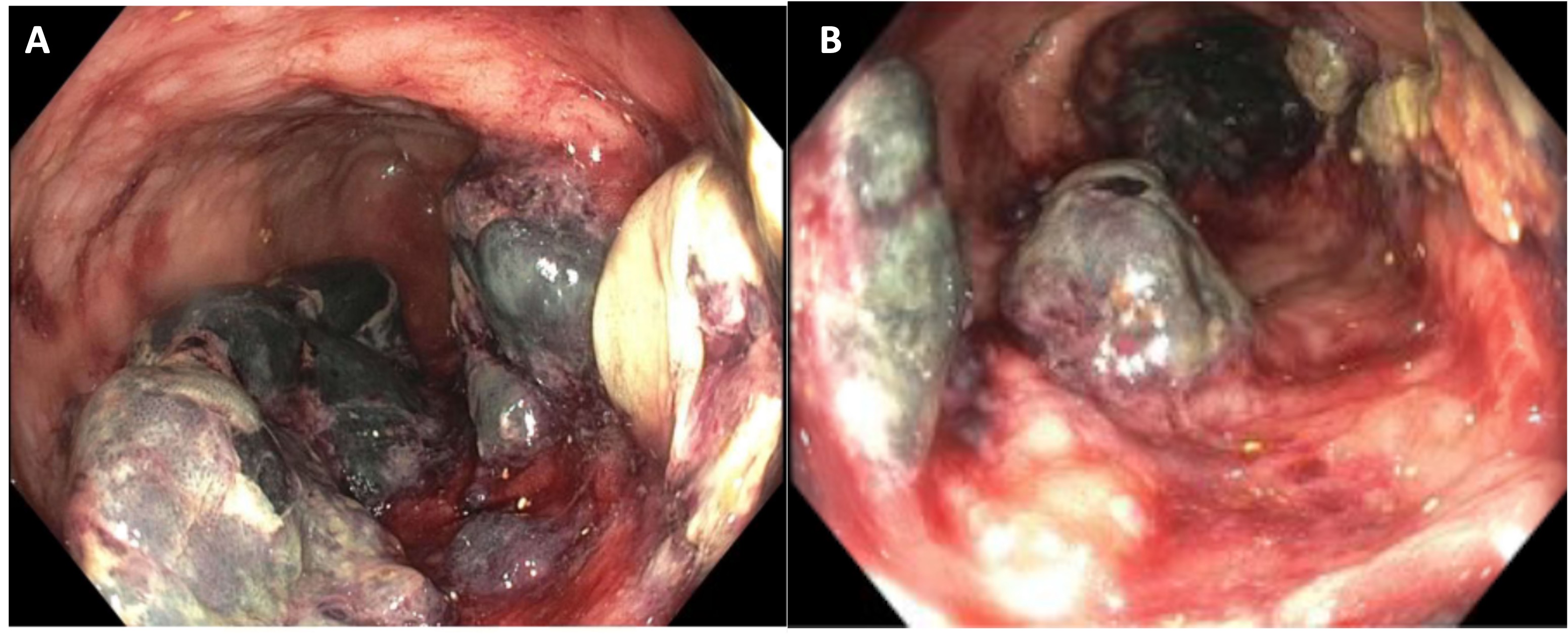
Figure: (A, B) Colonoscopy revealing venous blebs and hematomas with surrounding erythema and ulcerations
Disclosures:
Namrata Paladugu indicated no relevant financial relationships.
Hamid Ullah indicated no relevant financial relationships.
Satyapal Chahar indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Joydeep Chakraborty indicated no relevant financial relationships.
Namrata Paladugu, BS, MD, Hamid Ullah, MBBS, Satyapal Chahar, MD, Shou-jiang Tang, MD, Joydeep Chakraborty, MD. P2052 - An Unusual Cause of Hematochezia: Gastrointestinal Amyloidosis Manifesting as Venous Blebs and Submucosal Hematomas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

