Monday Poster Session
Category: Colon
P2091 - A Rare Case of Carbidopa-Levodopa Induced Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tatsiana Serhiyenia, MD
Einstein Healthcare Network
Bryn Mawr, PA
Presenting Author(s)
Award: Presidential Poster Award
Tatsiana Serhiyenia, MD1, Shikha Talwar, MD2, Steven Stanek, MD3, Yogesh Govil, MD4, Paul Belser, MD3
1Einstein Healthcare Network, Bryn Mawr, PA; 2Jefferson Einstein, Philadelphia, PA; 3Einstein Healthcare Network, East Norriton, PA; 4Einstein Medical Center, Philadelphia, PA
Introduction: Carbidopa-Levodopa is a widely used to treat Parkinson’s disease. There are many gastrointestinal side effects, however, carbidopa-Levodopa induced colitis is rarely seen with a limited number of documented cases.
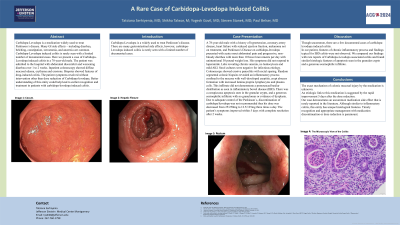
Case Description/Methods: A 78-year-old male with a history of hypertension, coronary artery disease, heart failure with reduced ejection fraction, melanoma not on treatment, and Parkinson’s Disease on carbidopa-levodopa presented with acute onset abdominal pain and progressive, non-bloody diarrhea with more than 10 bowel movements per day with unintentional 30 pound weight loss. His symptoms did not respond to loperamide. He was hemodynamically stable with labs revealing chronic anemia, no leukocytosis and mild AKI. Stool cultures were negative for infectious etiology. Colonoscopy showed erosive pancolitis with rectal sparing. Random segmental colonic biopsies revealed an inflammatory process confined to the mucosa with well-developed cryptitis, crypt abscess formation with increased lamina propria lymphocytes and plasma cells. This infiltrate did not demonstrate a pronounced basilar distribution as seen in inflammatory bowel disease (IBD). There was a conspicuous apoptosis seen in the granular crypts, and a generous eosinophilic infiltrate with no granulomas or evidence of dysplasia. Due to adequate control of his symptom, discontinuation of carbidopa/levodopa was not recommended thus his dose was decreased from 25/250mg to 12.5/125mg three times a day. The patient’s symptoms improved within 5 days with complete resolution of after 2 weeks.
Discussion: Though uncommon, there are a few documented cases of carbidopa-levodopa induced colitis. In our patient, features of chronic inflammatory process and findings typical for IBD colitis were not observed. We compared our findings with rare reports of Carbidopa-Levodopa associated colitis and found similar histologic features of apoptosis seen in the granular crypts and a generous eosinophilic infiltrate.
The exact mechanism of colonic mucosal injury by the medication is unknown. An etiologic link to this medication is suggested by the rapid improvement 5 days after the dose reduction.
Our case demonstrates an uncommon medication side effect that is rarely reported in the literature. Although similar to inflammatory colitis, this entity has unique histological features. Timely recognition and appropriate management with medication discontinuation or dose reduction is paramount.

Disclosures:
Tatsiana Serhiyenia, MD1, Shikha Talwar, MD2, Steven Stanek, MD3, Yogesh Govil, MD4, Paul Belser, MD3. P2091 - A Rare Case of Carbidopa-Levodopa Induced Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tatsiana Serhiyenia, MD1, Shikha Talwar, MD2, Steven Stanek, MD3, Yogesh Govil, MD4, Paul Belser, MD3
1Einstein Healthcare Network, Bryn Mawr, PA; 2Jefferson Einstein, Philadelphia, PA; 3Einstein Healthcare Network, East Norriton, PA; 4Einstein Medical Center, Philadelphia, PA
Introduction: Carbidopa-Levodopa is a widely used to treat Parkinson’s disease. There are many gastrointestinal side effects, however, carbidopa-Levodopa induced colitis is rarely seen with a limited number of documented cases.
Case Description/Methods: A 78-year-old male with a history of hypertension, coronary artery disease, heart failure with reduced ejection fraction, melanoma not on treatment, and Parkinson’s Disease on carbidopa-levodopa presented with acute onset abdominal pain and progressive, non-bloody diarrhea with more than 10 bowel movements per day with unintentional 30 pound weight loss. His symptoms did not respond to loperamide. He was hemodynamically stable with labs revealing chronic anemia, no leukocytosis and mild AKI. Stool cultures were negative for infectious etiology. Colonoscopy showed erosive pancolitis with rectal sparing. Random segmental colonic biopsies revealed an inflammatory process confined to the mucosa with well-developed cryptitis, crypt abscess formation with increased lamina propria lymphocytes and plasma cells. This infiltrate did not demonstrate a pronounced basilar distribution as seen in inflammatory bowel disease (IBD). There was a conspicuous apoptosis seen in the granular crypts, and a generous eosinophilic infiltrate with no granulomas or evidence of dysplasia. Due to adequate control of his symptom, discontinuation of carbidopa/levodopa was not recommended thus his dose was decreased from 25/250mg to 12.5/125mg three times a day. The patient’s symptoms improved within 5 days with complete resolution of after 2 weeks.
Discussion: Though uncommon, there are a few documented cases of carbidopa-levodopa induced colitis. In our patient, features of chronic inflammatory process and findings typical for IBD colitis were not observed. We compared our findings with rare reports of Carbidopa-Levodopa associated colitis and found similar histologic features of apoptosis seen in the granular crypts and a generous eosinophilic infiltrate.
The exact mechanism of colonic mucosal injury by the medication is unknown. An etiologic link to this medication is suggested by the rapid improvement 5 days after the dose reduction.
Our case demonstrates an uncommon medication side effect that is rarely reported in the literature. Although similar to inflammatory colitis, this entity has unique histological features. Timely recognition and appropriate management with medication discontinuation or dose reduction is paramount.

Figure: Hepatic flexure of the colon
Disclosures:
Tatsiana Serhiyenia indicated no relevant financial relationships.
Shikha Talwar indicated no relevant financial relationships.
Steven Stanek indicated no relevant financial relationships.
Yogesh Govil indicated no relevant financial relationships.
Paul Belser indicated no relevant financial relationships.
Tatsiana Serhiyenia, MD1, Shikha Talwar, MD2, Steven Stanek, MD3, Yogesh Govil, MD4, Paul Belser, MD3. P2091 - A Rare Case of Carbidopa-Levodopa Induced Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

