Monday Poster Session
Category: Colon
P2098 - A Mysterious Case of Abdominal Pain and Distention Revealing Eosinophilic Enteritis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HO
Haya Omeish, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Haya Omeish, MD1, Faisal Nimri, MD2, Ahmad Alomari, MD2, Abdulmalik Saleem, MD1, Jeffery Tang, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Eosinophilic Gastroenteritis (EGE) is a rare disorder marked by eosinophilic infiltration and peripheral eosinophilia. It can occur anywhere in the gastrointestinal tract without specific causes of eosinophilia. While its exact cause is unknown, hypersensitivity is significant. Symptoms include nausea, vomiting, abdominal pain, and weight loss. Diagnosis involves endoscopic biopsies, and prevalence is increasing with more endoscopic procedures. First-line treatment is steroids. We describe a case of diffuse abdominal pain leading to EGE diagnosis.
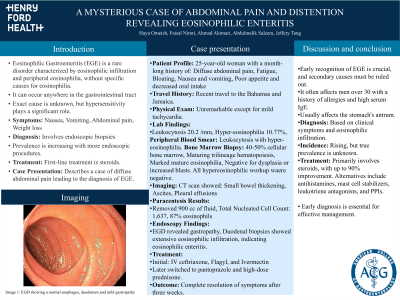
Case Description/Methods: A 25-year-old woman presented with a month-long history of diffuse abdominal pain, fatigue, bloating, nausea, vomiting, poor appetite, and decreased oral intake. She denied fever, weight loss, rash, or allergic disease history and reported recent travel to the Bahamas and Jamaica. Physical exam was unremarkable except for mild tachycardia. Labs showed leukocytosis with hyper-eosinophilia. Extensive workup ruled out secondary causes (Table-1). CT revealed small bowel thickening, ascites, and pleural effusions. Paracentesis removed 900 cc, showing a Total Nucleated Cell Count of 1,637 and 87% eosinophils. EGD showed gastropathy (Figure 1), and duodenal biopsies revealed extensive eosinophilic infiltration, suggesting eosinophilic enteritis. Treatment included IV ceftriaxone, Flagyl, and Ivermectin, later switching to pantoprazole and high-dose prednisone. Follow-up showed complete resolution of symptoms after three weeks.
Discussion: EGE is a rare condition with peripheral eosinophilia and gastrointestinal eosinophilic infiltration. Early suspicion is crucial, and secondary causes must be ruled out. EGE often affects men over 30 with allergy history and high serum IgE. It can impact any part of the digestive system, especially the stomach's antrum. Diagnosis involves gastrointestinal symptoms and eosinophilic infiltration. The incidence is rising, but true prevalence is unknown. Treatment, primarily steroids, shows up to 90% improvement. Alternatives include antihistamines, mast cell stabilizers, leukotriene antagonists, and PPIs. Early diagnosis is key.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Haya Omeish, MD1, Faisal Nimri, MD2, Ahmad Alomari, MD2, Abdulmalik Saleem, MD1, Jeffery Tang, MD1. P2098 - A Mysterious Case of Abdominal Pain and Distention Revealing Eosinophilic Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Eosinophilic Gastroenteritis (EGE) is a rare disorder marked by eosinophilic infiltration and peripheral eosinophilia. It can occur anywhere in the gastrointestinal tract without specific causes of eosinophilia. While its exact cause is unknown, hypersensitivity is significant. Symptoms include nausea, vomiting, abdominal pain, and weight loss. Diagnosis involves endoscopic biopsies, and prevalence is increasing with more endoscopic procedures. First-line treatment is steroids. We describe a case of diffuse abdominal pain leading to EGE diagnosis.
Case Description/Methods: A 25-year-old woman presented with a month-long history of diffuse abdominal pain, fatigue, bloating, nausea, vomiting, poor appetite, and decreased oral intake. She denied fever, weight loss, rash, or allergic disease history and reported recent travel to the Bahamas and Jamaica. Physical exam was unremarkable except for mild tachycardia. Labs showed leukocytosis with hyper-eosinophilia. Extensive workup ruled out secondary causes (Table-1). CT revealed small bowel thickening, ascites, and pleural effusions. Paracentesis removed 900 cc, showing a Total Nucleated Cell Count of 1,637 and 87% eosinophils. EGD showed gastropathy (Figure 1), and duodenal biopsies revealed extensive eosinophilic infiltration, suggesting eosinophilic enteritis. Treatment included IV ceftriaxone, Flagyl, and Ivermectin, later switching to pantoprazole and high-dose prednisone. Follow-up showed complete resolution of symptoms after three weeks.
Discussion: EGE is a rare condition with peripheral eosinophilia and gastrointestinal eosinophilic infiltration. Early suspicion is crucial, and secondary causes must be ruled out. EGE often affects men over 30 with allergy history and high serum IgE. It can impact any part of the digestive system, especially the stomach's antrum. Diagnosis involves gastrointestinal symptoms and eosinophilic infiltration. The incidence is rising, but true prevalence is unknown. Treatment, primarily steroids, shows up to 90% improvement. Alternatives include antihistamines, mast cell stabilizers, leukotriene antagonists, and PPIs. Early diagnosis is key.

Figure: EGD showing a normal esophagus, duodenum and gastropathy
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Haya Omeish indicated no relevant financial relationships.
Faisal Nimri indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Jeffery Tang indicated no relevant financial relationships.
Haya Omeish, MD1, Faisal Nimri, MD2, Ahmad Alomari, MD2, Abdulmalik Saleem, MD1, Jeffery Tang, MD1. P2098 - A Mysterious Case of Abdominal Pain and Distention Revealing Eosinophilic Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
