Monday Poster Session
Category: Colorectal Cancer Prevention
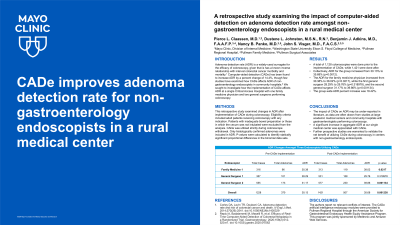
P2129 - A Retrospective Study Examining the Impact of Computer-Aided Detection on Adenoma Detection Rate Amongst Non-Gastroenterology Endoscopists in a Rural Medical Center
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Pierce L. Claassen, MD
Washington State University Elson S. Floyd College of Medicine
Phoenix, AZ
Presenting Author(s)
Pierce L. Claassen, MD1, Dustene L. Johnston, MSN, RN2, Benjamin J. Adkins, MD3, Nancy B. Panko, MD4, John S. Visger, MD5
1Washington State University Elson S. Floyd College of Medicine, Phoenix, AZ; 2Pullman Regional Hospital, Pullman, WA; 3Pullman Regional Hospital, Pullman Family Medicine, Pullman, WA; 4Pullman Regional Hospital, Pullman Surgical Associates, Pullman, WA; 5Pullman Regional Hospital, Pullman Surgical Associates, Washington State University Elson S. Floyd College of Medicine, Pullman, WA
Introduction: Adenoma detection rate (ADR) is a widely-used surrogate for the efficacy of colonoscopy, given that is has a known inverse relationship with interval colorectal cancer morbidity and mortality. Computer-aided detection (CADe) has been found to increase ADR by a percent change of 14.4%, though few studies have examined how CADe affects ADR of non-gastroenterology endoscopists in community hospitals. We sought to investigate how the implementation of CADe affects ADR at a single Critical Access Hospital with one family medicine physician and two general surgeons performing colonoscopy.
Methods: This retrospective study examined changes in ADR after implementation of CADe during colonoscopy. Eligibility criteria included adult patients receiving colonoscopy with any indication. Patients with inadequate bowel preparation or those in which the cecum was not intubated were excluded from the analysis. CADe was utilized strictly during colonoscope withdrawal. Only histologically confirmed adenomas were included in ADR. P-values were calculated to identify statically significant proportional differences in the binomial data sets.
Results: A total of 1,128 colonoscopies were done prior to the implementation of CADe, while 1,421 were done after. Collectively, ADR for the group increased from 30.13% to 35.68% (p=0.0012). The ADR for the family medicine physician increased from 30.38% to 38.02% (p=0.0217), while the first general surgeon 28.29% to 29.76% (p=0.318978), and the second general surgeon 31.17% to 39.86% (p=0.001134). The group-wide ADR percent increase was 18.42%.
Discussion: The impact of CADe on ADR may be under-reported in literature, as data are often drawn from studies at large academic medical centers and community hospitals with gastroenterologists performing colonoscopy. The group-wide and individual increases in ADR after implementing CADe at our Critical Access Hospital necessitate that further prospective studies are warranted to validate the net benefit of utilizing CADe during colonoscopy in centers with non-gastroenterology endoscopists.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pierce L. Claassen, MD1, Dustene L. Johnston, MSN, RN2, Benjamin J. Adkins, MD3, Nancy B. Panko, MD4, John S. Visger, MD5. P2129 - A Retrospective Study Examining the Impact of Computer-Aided Detection on Adenoma Detection Rate Amongst Non-Gastroenterology Endoscopists in a Rural Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington State University Elson S. Floyd College of Medicine, Phoenix, AZ; 2Pullman Regional Hospital, Pullman, WA; 3Pullman Regional Hospital, Pullman Family Medicine, Pullman, WA; 4Pullman Regional Hospital, Pullman Surgical Associates, Pullman, WA; 5Pullman Regional Hospital, Pullman Surgical Associates, Washington State University Elson S. Floyd College of Medicine, Pullman, WA
Introduction: Adenoma detection rate (ADR) is a widely-used surrogate for the efficacy of colonoscopy, given that is has a known inverse relationship with interval colorectal cancer morbidity and mortality. Computer-aided detection (CADe) has been found to increase ADR by a percent change of 14.4%, though few studies have examined how CADe affects ADR of non-gastroenterology endoscopists in community hospitals. We sought to investigate how the implementation of CADe affects ADR at a single Critical Access Hospital with one family medicine physician and two general surgeons performing colonoscopy.
Methods: This retrospective study examined changes in ADR after implementation of CADe during colonoscopy. Eligibility criteria included adult patients receiving colonoscopy with any indication. Patients with inadequate bowel preparation or those in which the cecum was not intubated were excluded from the analysis. CADe was utilized strictly during colonoscope withdrawal. Only histologically confirmed adenomas were included in ADR. P-values were calculated to identify statically significant proportional differences in the binomial data sets.
Results: A total of 1,128 colonoscopies were done prior to the implementation of CADe, while 1,421 were done after. Collectively, ADR for the group increased from 30.13% to 35.68% (p=0.0012). The ADR for the family medicine physician increased from 30.38% to 38.02% (p=0.0217), while the first general surgeon 28.29% to 29.76% (p=0.318978), and the second general surgeon 31.17% to 39.86% (p=0.001134). The group-wide ADR percent increase was 18.42%.
Discussion: The impact of CADe on ADR may be under-reported in literature, as data are often drawn from studies at large academic medical centers and community hospitals with gastroenterologists performing colonoscopy. The group-wide and individual increases in ADR after implementing CADe at our Critical Access Hospital necessitate that further prospective studies are warranted to validate the net benefit of utilizing CADe during colonoscopy in centers with non-gastroenterology endoscopists.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pierce Claassen indicated no relevant financial relationships.
Dustene Johnston indicated no relevant financial relationships.
Benjamin Adkins indicated no relevant financial relationships.
Nancy Panko indicated no relevant financial relationships.
John Visger indicated no relevant financial relationships.
Pierce L. Claassen, MD1, Dustene L. Johnston, MSN, RN2, Benjamin J. Adkins, MD3, Nancy B. Panko, MD4, John S. Visger, MD5. P2129 - A Retrospective Study Examining the Impact of Computer-Aided Detection on Adenoma Detection Rate Amongst Non-Gastroenterology Endoscopists in a Rural Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
