Monday Poster Session
Category: Colorectal Cancer Prevention
P2130 - Improving FITness: Increasing Colorectal Cancer Screening Rates in Average-Risk Veterans Aged 45-49 in Southeast Louisiana
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DP
Duncan Pearce, MD
Tulane Medical Center
New Orleans, LA
Presenting Author(s)
Duncan Pearce, MD1, Ryan Burden, MD1, Marla Stewart, RN2, Albert Jang, MD1, Caitlin Martin-Klinger, MD2, Leela Nayak, MD2, Anthony Marsh, MD2, Tanya Payton, 2, William Kirsch, 2
1Tulane Medical Center, New Orleans, LA; 2VA Southeast Louisiana Health Care, New Orleans, LA
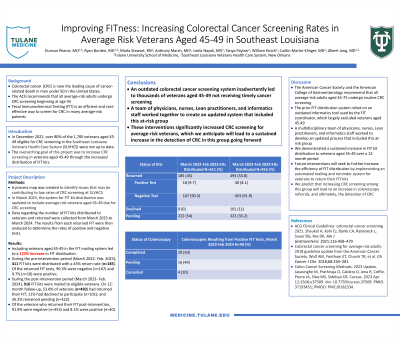
Introduction: Colorectal cancer (CRC) is now the leading cause of cancer-related death in men under 50 in the United States. In December 2022, over 80% of the 1,700 veterans aged 45-49 eligible for CRC screening in the Southeast Louisiana Veterans Health Care System (SLVHCS) were not up to date. Fecal Immunochemical Testing (FIT) is an efficient and cost-effective way to screen for CRC in many average-risk patients. The overarching goal of this project was to increase CRC screening in veterans aged 45-49 through the increased distribution of FIT kits.
Methods: A process map was created to identify issues that may be contributing to low rates of CRC screening at SLVHCS. The baseline process for sending FIT kits to veterans did not include those aged 45-49 due to the use of an outdated informatics tool. In March 2023, the system for FIT distribution was updated to include average-risk veterans aged 45-49 due for CRC screening. Data regarding the number of FIT kits distributed to veterans and returned were collected from March 2022 to February 2024. The results from each returned FIT were then analyzed to determine the rates of positive and negative tests.
Results: Including veterans aged 45-49 in the FIT mailing system led to a 123% increase in FIT distribution. During the pre-intervention period (March 2022-Feb. 2023), 411 FIT kits were distributed with a 45% return rate (n=185). Of the returned FIT tests, 90.3% were negative (n=167) and 9.7% (n=18) were positive. During the post-intervention period (March 2023-Feb. 2024), 916 FIT kits were mailed to eligible veterans. On 12-month follow-up, 53.8% of veterans (n=493) had returned their FIT; 11% had declined to participate (n=101); and 35.2% remained pending (n=322). Of the veterans who returned their FIT, 91.9% were negative (n=453) and 8.1% were positive (n=40).
Discussion: The prior FIT distribution system relied on an outdated informatics tool used by the FIT coordinator, which largely excluded veterans aged 45-49. A multidisciplinary team of physicians, nurses, Lean practitioners, and informatics staff worked to develop an updated process that included this at-risk group. Through this process modification, we demonstrated an increase in FIT distribution to veterans aged 45-49 over a 12-month period. Future interventions will seek to further increase CRC screening rates by implementing an automated mailing and nursing reminder system for the distribution of FIT kits to veterans.
Disclosures:
Duncan Pearce, MD1, Ryan Burden, MD1, Marla Stewart, RN2, Albert Jang, MD1, Caitlin Martin-Klinger, MD2, Leela Nayak, MD2, Anthony Marsh, MD2, Tanya Payton, 2, William Kirsch, 2. P2130 - Improving FITness: Increasing Colorectal Cancer Screening Rates in Average-Risk Veterans Aged 45-49 in Southeast Louisiana, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tulane Medical Center, New Orleans, LA; 2VA Southeast Louisiana Health Care, New Orleans, LA
Introduction: Colorectal cancer (CRC) is now the leading cause of cancer-related death in men under 50 in the United States. In December 2022, over 80% of the 1,700 veterans aged 45-49 eligible for CRC screening in the Southeast Louisiana Veterans Health Care System (SLVHCS) were not up to date. Fecal Immunochemical Testing (FIT) is an efficient and cost-effective way to screen for CRC in many average-risk patients. The overarching goal of this project was to increase CRC screening in veterans aged 45-49 through the increased distribution of FIT kits.
Methods: A process map was created to identify issues that may be contributing to low rates of CRC screening at SLVHCS. The baseline process for sending FIT kits to veterans did not include those aged 45-49 due to the use of an outdated informatics tool. In March 2023, the system for FIT distribution was updated to include average-risk veterans aged 45-49 due for CRC screening. Data regarding the number of FIT kits distributed to veterans and returned were collected from March 2022 to February 2024. The results from each returned FIT were then analyzed to determine the rates of positive and negative tests.
Results: Including veterans aged 45-49 in the FIT mailing system led to a 123% increase in FIT distribution. During the pre-intervention period (March 2022-Feb. 2023), 411 FIT kits were distributed with a 45% return rate (n=185). Of the returned FIT tests, 90.3% were negative (n=167) and 9.7% (n=18) were positive. During the post-intervention period (March 2023-Feb. 2024), 916 FIT kits were mailed to eligible veterans. On 12-month follow-up, 53.8% of veterans (n=493) had returned their FIT; 11% had declined to participate (n=101); and 35.2% remained pending (n=322). Of the veterans who returned their FIT, 91.9% were negative (n=453) and 8.1% were positive (n=40).
Discussion: The prior FIT distribution system relied on an outdated informatics tool used by the FIT coordinator, which largely excluded veterans aged 45-49. A multidisciplinary team of physicians, nurses, Lean practitioners, and informatics staff worked to develop an updated process that included this at-risk group. Through this process modification, we demonstrated an increase in FIT distribution to veterans aged 45-49 over a 12-month period. Future interventions will seek to further increase CRC screening rates by implementing an automated mailing and nursing reminder system for the distribution of FIT kits to veterans.
Disclosures:
Duncan Pearce indicated no relevant financial relationships.
Ryan Burden indicated no relevant financial relationships.
Marla Stewart indicated no relevant financial relationships.
Albert Jang indicated no relevant financial relationships.
Caitlin Martin-Klinger indicated no relevant financial relationships.
Leela Nayak indicated no relevant financial relationships.
Anthony Marsh indicated no relevant financial relationships.
Tanya Payton indicated no relevant financial relationships.
William Kirsch indicated no relevant financial relationships.
Duncan Pearce, MD1, Ryan Burden, MD1, Marla Stewart, RN2, Albert Jang, MD1, Caitlin Martin-Klinger, MD2, Leela Nayak, MD2, Anthony Marsh, MD2, Tanya Payton, 2, William Kirsch, 2. P2130 - Improving FITness: Increasing Colorectal Cancer Screening Rates in Average-Risk Veterans Aged 45-49 in Southeast Louisiana, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
