Monday Poster Session
Category: Colorectal Cancer Prevention
P2137 - Assessing Rates of Colorectal Cancer Diagnosis and Survival With Colonoscopies in the Elderly: A Real-World Analysis From a Large Integrated Health System
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JG
Jacob Gries, MD, MSc
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Jacob Gries, MD, MSc1, Emely Pimentel, MD2, Candace Miyaki, DO2, Abuzar Siraj, MD2, Malak S. Al-Bitar, MD1, Hema M. Srinivasan, 2, Andrea Berger, 2, David L. Diehl, MD2
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA
Introduction: Guidance is limited on colorectal cancer (CRC) screening or surveillance with colonoscopy in patients over 74 who have adhered to CRC screening guidelines. This retrospective study assessed the incidence of CRC and survival related to colonoscopies in patients older than 74.
Methods: This IRB-approved study from a large academic medical system identified patients over 74 who had at least 2 colonoscopies before 75 years, per USPSTF guidelines. Patients diagnosed with CRC before 75 were excluded. Patients were divided into those with a colonoscopy after 74 and those without. Data on CRC diagnosis, colonoscopy indication, age at death, causes of death, comorbidities, and demographics were collected. Colonoscopy indications included screening, surveillance, GI symptoms, abnormal imaging, and positive stool tests (i.e., hemoccult, FIT). Modified Charlson Comorbidity Indices (CCI, excluding HIV/AIDS) assessed baseline health at the time of colonoscopy.
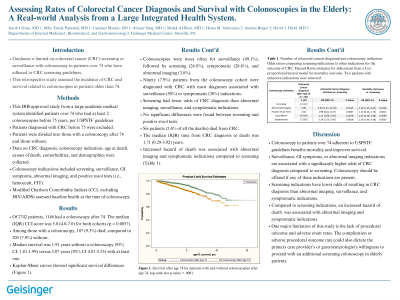
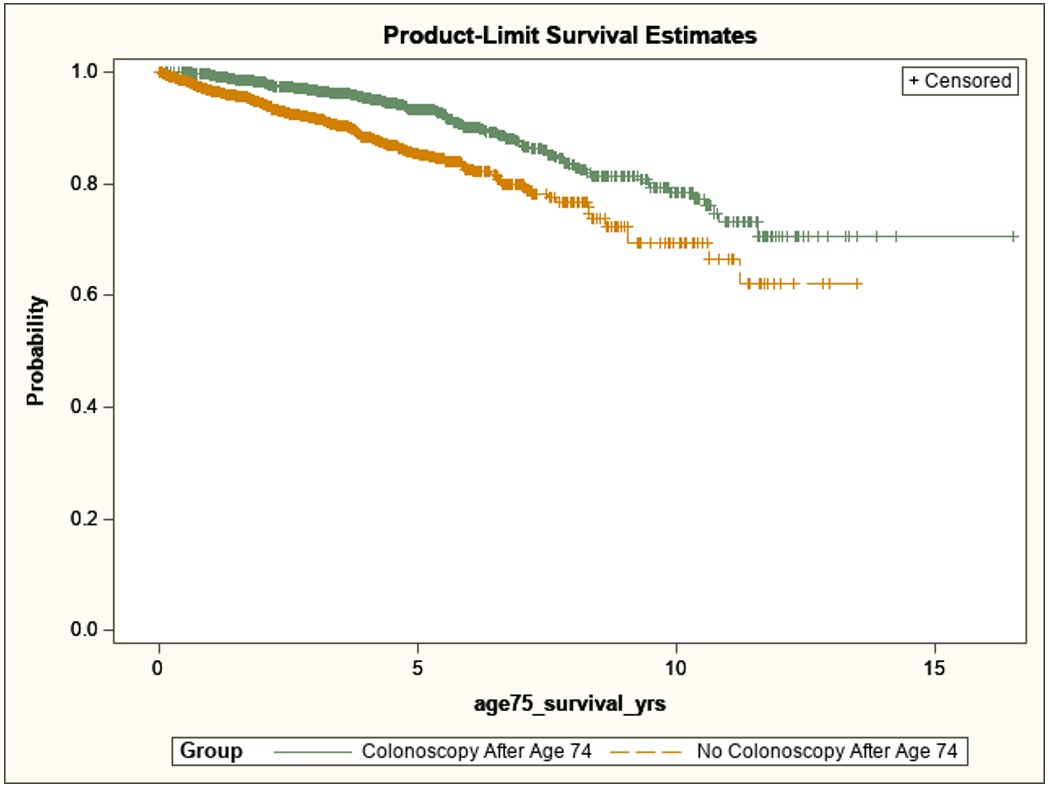
Results: Of 2742 patients, 1146 had a colonoscopy after 74. The median (IQR) CCI score was 5.0 (4.0-7.0) for both cohorts (p = 0.0057). Among those with a colonoscopy, 107 (9.3%) died, compared to 205 (7.9%) without. Median survival was 1.91 years without a colonoscopy (95% CI: 1.81-1.99) versus 5.07 years (95% CI 4.81-5.25) with at least one. Kaplan-Meier curves showed significant survival differences (Figure 1). Colonoscopies were most often for surveillance (49.1%), followed by screening (24.8%), symptomatic (20.6%), and abnormal imaging (3.0%). Ninety (7.9%) patients from the colonoscopy cohort were diagnosed with CRC with most diagnoses associated with surveillance (50%) or symptomatic (30%) indications. Screening had lower odds of CRC diagnosis than abnormal imaging, surveillance, and symptomatic indications. No significant differences were found between screening and positive stool tests. Six patients (5.6% of all the deaths) died from CRC. The median (IQR) time from CRC diagnosis to death was 1.71 (0.29-3.92) years. Increased hazard of death was associated with abnormal imaging and symptomatic indications compared to screening (Table 1).
Discussion: Colonoscopy in patients over 74 adherent to USPSTF guidelines benefits mortality and improves survival. Surveillance, GI symptoms, or abnormal imaging indications are associated with a significantly higher odds of CRC diagnosis compared to screening. Colonoscopy should be offered if any of these indications are present.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacob Gries, MD, MSc1, Emely Pimentel, MD2, Candace Miyaki, DO2, Abuzar Siraj, MD2, Malak S. Al-Bitar, MD1, Hema M. Srinivasan, 2, Andrea Berger, 2, David L. Diehl, MD2. P2137 - Assessing Rates of Colorectal Cancer Diagnosis and Survival With Colonoscopies in the Elderly: A Real-World Analysis From a Large Integrated Health System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA
Introduction: Guidance is limited on colorectal cancer (CRC) screening or surveillance with colonoscopy in patients over 74 who have adhered to CRC screening guidelines. This retrospective study assessed the incidence of CRC and survival related to colonoscopies in patients older than 74.
Methods: This IRB-approved study from a large academic medical system identified patients over 74 who had at least 2 colonoscopies before 75 years, per USPSTF guidelines. Patients diagnosed with CRC before 75 were excluded. Patients were divided into those with a colonoscopy after 74 and those without. Data on CRC diagnosis, colonoscopy indication, age at death, causes of death, comorbidities, and demographics were collected. Colonoscopy indications included screening, surveillance, GI symptoms, abnormal imaging, and positive stool tests (i.e., hemoccult, FIT). Modified Charlson Comorbidity Indices (CCI, excluding HIV/AIDS) assessed baseline health at the time of colonoscopy.
Results: Of 2742 patients, 1146 had a colonoscopy after 74. The median (IQR) CCI score was 5.0 (4.0-7.0) for both cohorts (p = 0.0057). Among those with a colonoscopy, 107 (9.3%) died, compared to 205 (7.9%) without. Median survival was 1.91 years without a colonoscopy (95% CI: 1.81-1.99) versus 5.07 years (95% CI 4.81-5.25) with at least one. Kaplan-Meier curves showed significant survival differences (Figure 1). Colonoscopies were most often for surveillance (49.1%), followed by screening (24.8%), symptomatic (20.6%), and abnormal imaging (3.0%). Ninety (7.9%) patients from the colonoscopy cohort were diagnosed with CRC with most diagnoses associated with surveillance (50%) or symptomatic (30%) indications. Screening had lower odds of CRC diagnosis than abnormal imaging, surveillance, and symptomatic indications. No significant differences were found between screening and positive stool tests. Six patients (5.6% of all the deaths) died from CRC. The median (IQR) time from CRC diagnosis to death was 1.71 (0.29-3.92) years. Increased hazard of death was associated with abnormal imaging and symptomatic indications compared to screening (Table 1).
Discussion: Colonoscopy in patients over 74 adherent to USPSTF guidelines benefits mortality and improves survival. Surveillance, GI symptoms, or abnormal imaging indications are associated with a significantly higher odds of CRC diagnosis compared to screening. Colonoscopy should be offered if any of these indications are present.
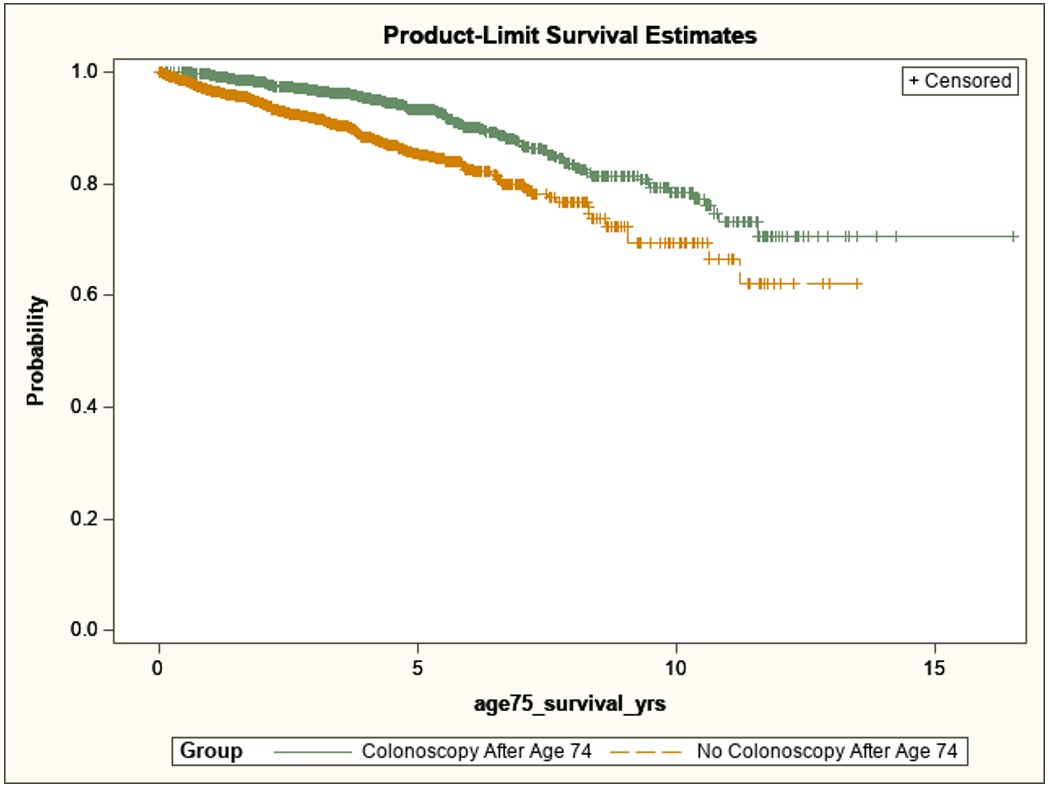
Figure: Figure 1. Survival after age 74 for patients with and without colonoscopies after age 74, log-rank test p-value < .0001.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacob Gries indicated no relevant financial relationships.
Emely Pimentel indicated no relevant financial relationships.
Candace Miyaki indicated no relevant financial relationships.
Abuzar Siraj indicated no relevant financial relationships.
Malak Al-Bitar indicated no relevant financial relationships.
Hema Srinivasan indicated no relevant financial relationships.
Andrea Berger indicated no relevant financial relationships.
David Diehl: Castle Biosciences – Consultant.
Jacob Gries, MD, MSc1, Emely Pimentel, MD2, Candace Miyaki, DO2, Abuzar Siraj, MD2, Malak S. Al-Bitar, MD1, Hema M. Srinivasan, 2, Andrea Berger, 2, David L. Diehl, MD2. P2137 - Assessing Rates of Colorectal Cancer Diagnosis and Survival With Colonoscopies in the Elderly: A Real-World Analysis From a Large Integrated Health System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

