Monday Poster Session
Category: Colorectal Cancer Prevention
P2141 - Differences in Lynch Syndrome Surveillance Colonoscopy by Mismatch Repair Gene Type: Experiences From a Mid-Atlantic Healthcare System
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Joseph O. Atarere, MD, MPH
MedStar Union Memorial Hospital
Baltimore, MD
Presenting Author(s)
Joseph Atarere, MD, MPH1, Boniface Mensah, MBChB, MPH1, Mariah Malak Bilalaga, MD1, Ramya Vasireddy, MBBS1, Ted Akhiwu, MBBS, MPH1, Greeshma Gaddipati, MBBS1, Simardeep Singh, MBBS1, Stephanie M. Woo, MD2, Priyanka Kanth, MD2
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Lynch syndrome (LS) is caused by germline mutations in the mismatch repair (MMR) system. Mutations in MLH1 and MSH2 account for 70%-90% of LS and carriers have the highest risk of developing colorectal cancer (CRC). Screening colonoscopies are recommended for all individuals with LS starting at age 20- 25, with considerations to begin at ages 30 and 35 years in those with MSH6 and PMS2 respectively. Current guidelines recommend follow-up colonoscopies every 1-2 years, regardless of MMR gene type. In this study, we compared the time from baseline colonoscopy to detection of a high-risk lesion or CRC to determine if a different follow-up schedule may be appropriate for certain MMR types.
Methods: We extracted data from a retrospective cohort of patients with a germline diagnosis of LS who received colonoscopies between April 13th, 2005, and February 27th, 2024. Only those with normal baseline colonoscopy findings were included. We had a composite outcome of CRC or high-risk lesion [adenoma, sessile serrated polyp (SSP)] detection on follow-up colonoscopies. The primary independent variable was germline mutation (MLH1, MSH2, MSH6, PMS2 and EPCAM). We plotted Kaplan-Meier (KM) survival curves for the length of time from baseline colonoscopy till study outcome occurrence by MMR subtype, comparing the survivor functions with log-rank tests. We described the relationship between MMR subtype and time to study endpoint using an age and sex-adjusted cox-proportional hazard model.
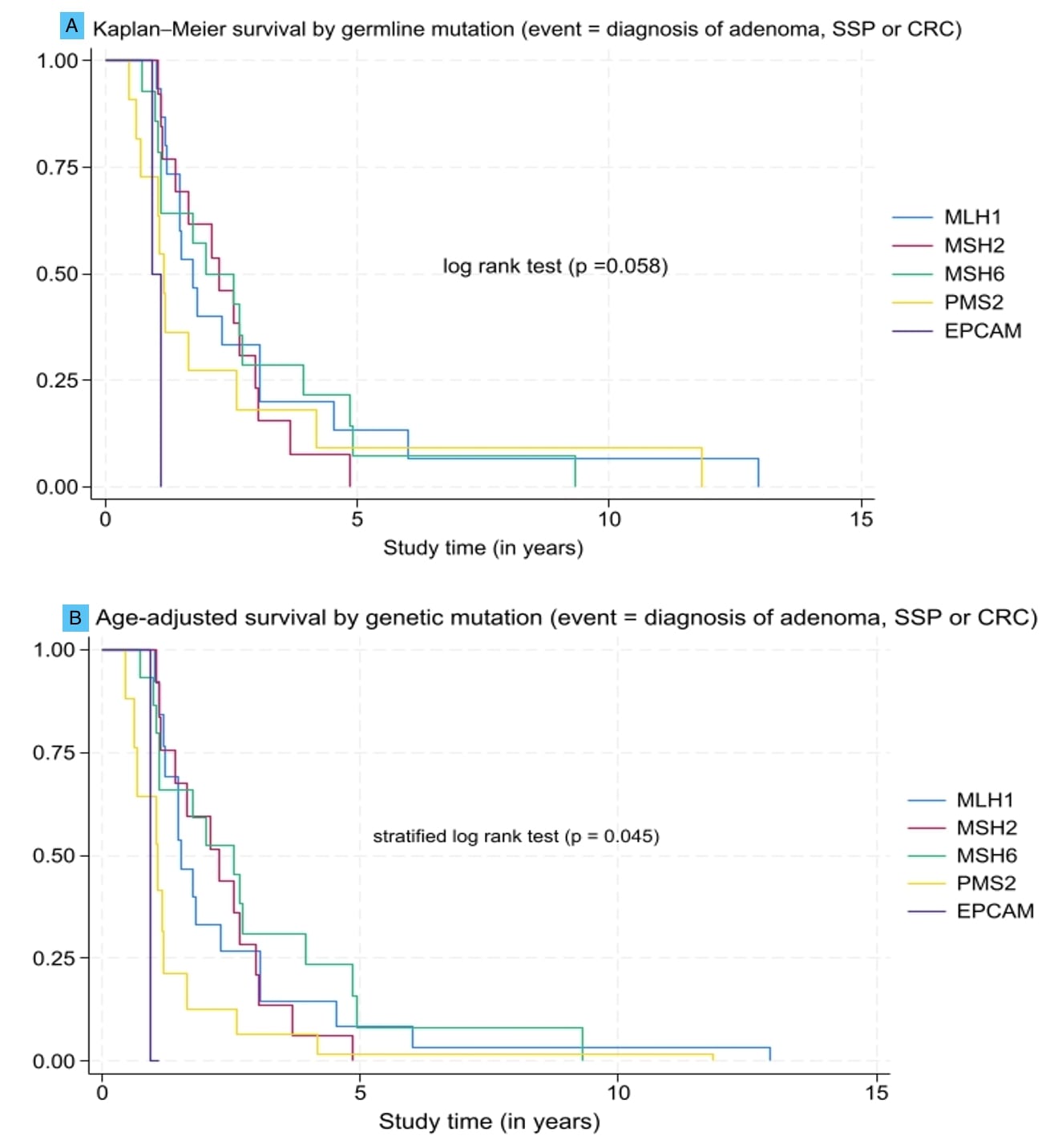
Results: We included a total of 96 patients in this study of which 22 (22.9%) had MLH1 mutations. Most (80.2%) of the population were female and the mean number of colonoscopies was 3. The average duration of follow-up was highest for MSH2 (64 months) and lowest for PMS2 (24 months) (Table 1). The age-adjusted KM survival showed a significant difference in time to study outcome by mutation type (p = 0.045) (fig 1). In the adjusted cox-proportional hazard model, compared to MLH1, there was no difference in the detection of adenoma, SSP or CRC among patients with MSH2, MSH6, and PMS2 mutations.
Discussion: Patients with MSH2 and MLH1 had the longest duration of follow-up which is reassuring as they have the highest risk of developing CRC. Interestingly, no differences were noted in the development of precancerous lesions and CRC between MMR subtypes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Atarere, MD, MPH1, Boniface Mensah, MBChB, MPH1, Mariah Malak Bilalaga, MD1, Ramya Vasireddy, MBBS1, Ted Akhiwu, MBBS, MPH1, Greeshma Gaddipati, MBBS1, Simardeep Singh, MBBS1, Stephanie M. Woo, MD2, Priyanka Kanth, MD2. P2141 - Differences in Lynch Syndrome Surveillance Colonoscopy by Mismatch Repair Gene Type: Experiences From a Mid-Atlantic Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Lynch syndrome (LS) is caused by germline mutations in the mismatch repair (MMR) system. Mutations in MLH1 and MSH2 account for 70%-90% of LS and carriers have the highest risk of developing colorectal cancer (CRC). Screening colonoscopies are recommended for all individuals with LS starting at age 20- 25, with considerations to begin at ages 30 and 35 years in those with MSH6 and PMS2 respectively. Current guidelines recommend follow-up colonoscopies every 1-2 years, regardless of MMR gene type. In this study, we compared the time from baseline colonoscopy to detection of a high-risk lesion or CRC to determine if a different follow-up schedule may be appropriate for certain MMR types.
Methods: We extracted data from a retrospective cohort of patients with a germline diagnosis of LS who received colonoscopies between April 13th, 2005, and February 27th, 2024. Only those with normal baseline colonoscopy findings were included. We had a composite outcome of CRC or high-risk lesion [adenoma, sessile serrated polyp (SSP)] detection on follow-up colonoscopies. The primary independent variable was germline mutation (MLH1, MSH2, MSH6, PMS2 and EPCAM). We plotted Kaplan-Meier (KM) survival curves for the length of time from baseline colonoscopy till study outcome occurrence by MMR subtype, comparing the survivor functions with log-rank tests. We described the relationship between MMR subtype and time to study endpoint using an age and sex-adjusted cox-proportional hazard model.
Results: We included a total of 96 patients in this study of which 22 (22.9%) had MLH1 mutations. Most (80.2%) of the population were female and the mean number of colonoscopies was 3. The average duration of follow-up was highest for MSH2 (64 months) and lowest for PMS2 (24 months) (Table 1). The age-adjusted KM survival showed a significant difference in time to study outcome by mutation type (p = 0.045) (fig 1). In the adjusted cox-proportional hazard model, compared to MLH1, there was no difference in the detection of adenoma, SSP or CRC among patients with MSH2, MSH6, and PMS2 mutations.
Discussion: Patients with MSH2 and MLH1 had the longest duration of follow-up which is reassuring as they have the highest risk of developing CRC. Interestingly, no differences were noted in the development of precancerous lesions and CRC between MMR subtypes.
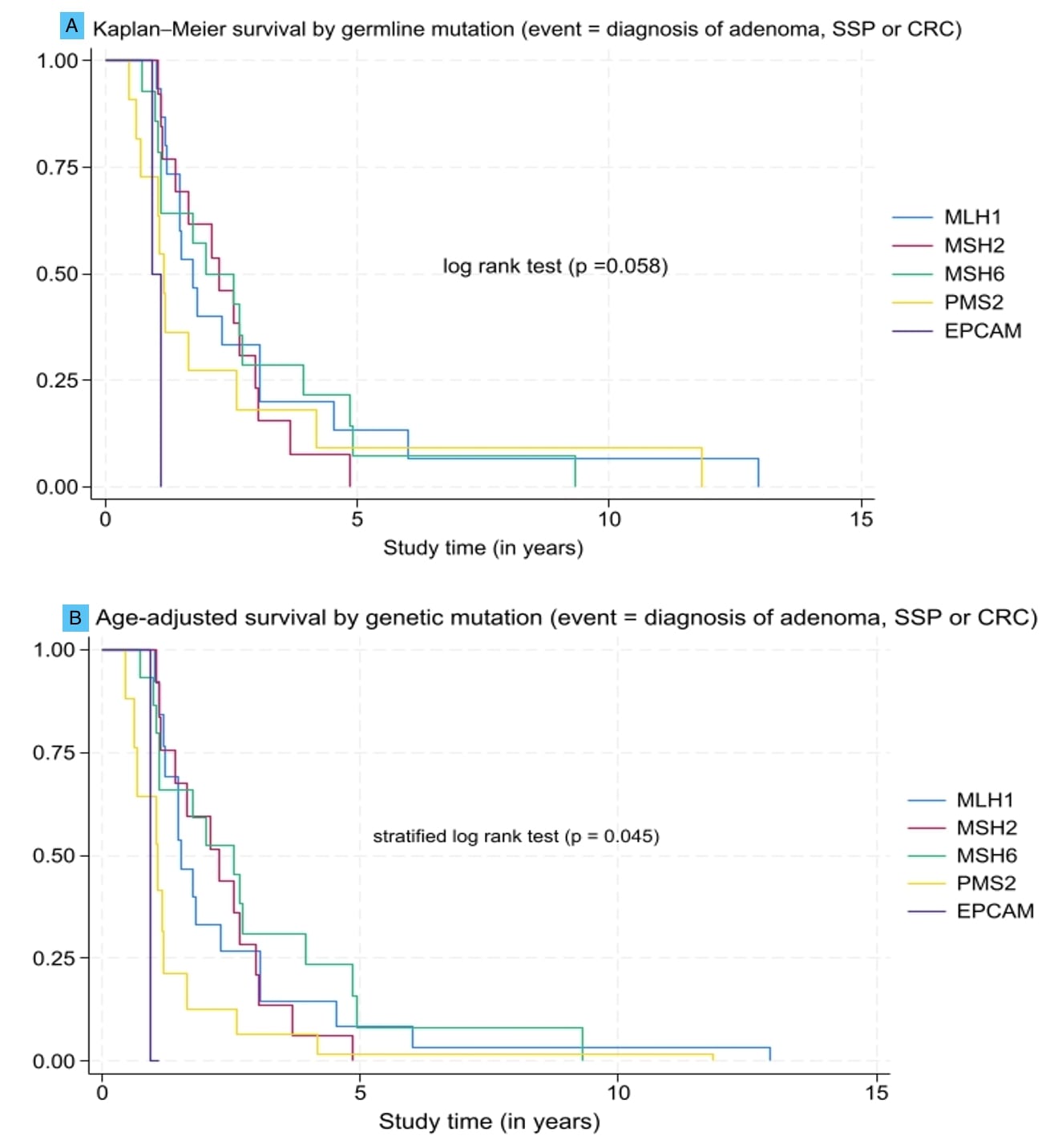
Figure: Figure 1: Kaplan Meier survival graphs showing time to first diagnosis of adenoma, sessile serrated polyp (SSP) or colorectal cancer (CRC), stratified by germline mutation (A) unadjusted and (B) adjusted for age.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Atarere indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Mariah Malak Bilalaga indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Ted Akhiwu indicated no relevant financial relationships.
Greeshma Gaddipati indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Stephanie Woo indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Joseph Atarere, MD, MPH1, Boniface Mensah, MBChB, MPH1, Mariah Malak Bilalaga, MD1, Ramya Vasireddy, MBBS1, Ted Akhiwu, MBBS, MPH1, Greeshma Gaddipati, MBBS1, Simardeep Singh, MBBS1, Stephanie M. Woo, MD2, Priyanka Kanth, MD2. P2141 - Differences in Lynch Syndrome Surveillance Colonoscopy by Mismatch Repair Gene Type: Experiences From a Mid-Atlantic Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
