Monday Poster Session
Category: Endoscopy Video Forum
P2170 - Endoscopic Ultrasound-Guided Gastroenterostomy: An Animated Educational Video Review
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arjun Chatterjee, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Arjun Chatterjee, MD1, Raj Jessica Thomas, MD2, Zehra Naseem, MD1, Amandeep Singh, MD2, Prabhleen Chahal, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Akron General, Akron, OH
Introduction: Gastric outlet obstruction (GOO) has been traditionally treated surgically or with duodenal stent. Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has recently emerged as an alternative minimally invasive technique for managing benign and malignant GOO. This animated educational video reviews three EUS-GE techniques: direct, EUS-guided balloon-occluded gastrojejunostomy bypass (EPASS), and orojejunal tube-facilitated contrast-enhanced method.
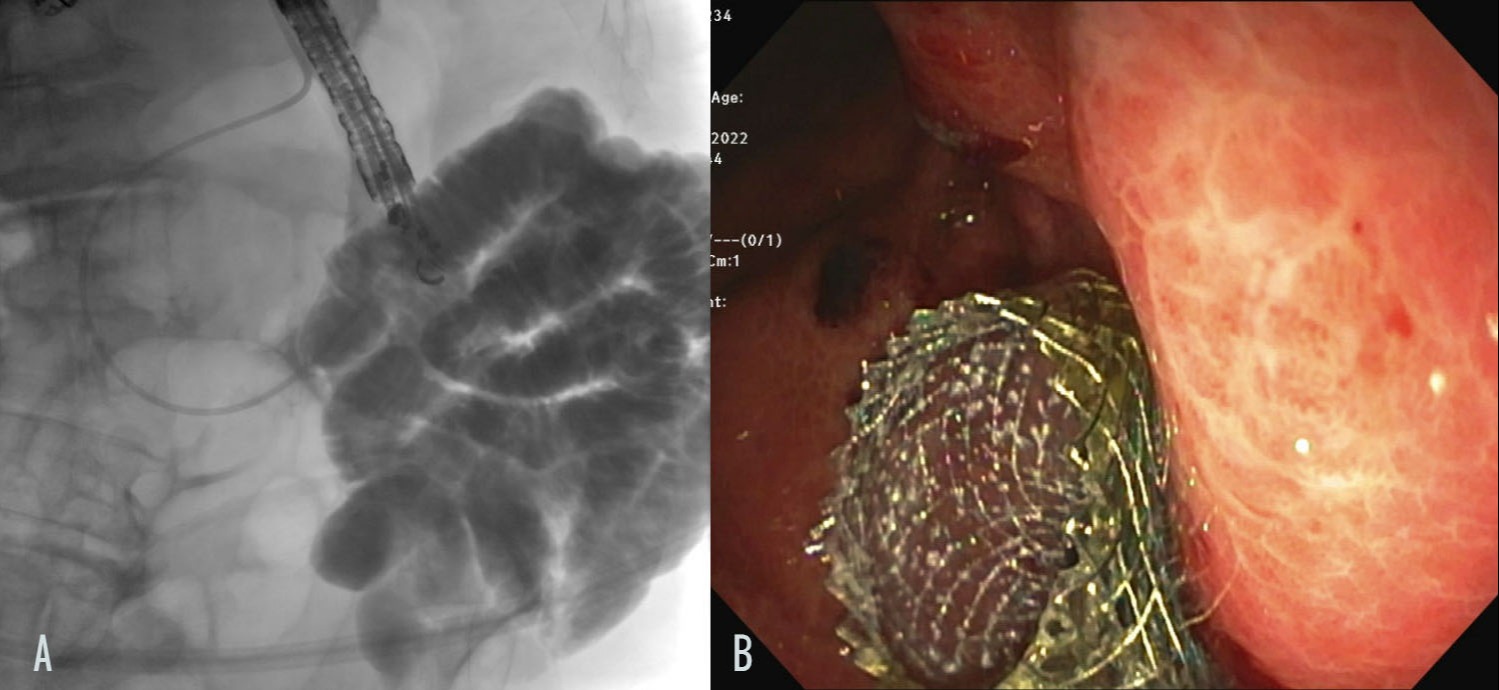
Case Description/Methods: An 82-year-old man with a malignant bladder tumor presented with worsening nausea, vomiting, and abdominal cramping. Computed tomography scan showed duodenal wall thickening causing GOO. Endoscopy revealed severe stenosis of second part of duodenum. Using orojejunal tube-facilitated contrast-enhanced EUS-GE technique, a lumen apposing metal stent (LAMS) was placed to create EUS-GE. (Figure 1). His symptoms resolved completely, and a small bowel follow-through showed GOO resolution and a patent gastro-jejunal stent.
Discussion: Direct EUS-GE method: a linear endoscope is used to identify the jejunal or distal duodenum loop. Under EUS-guidance, a 19-gauge needle is used to instill a 250cc contrast mixture, followed by deploying a cautery-enhanced LAMS. Safety checks ensure proper alignment. Orojejunal tube-facilitated contrast-enhanced technique: standard or therapeutic endoscope is advanced to the obstruction site. If the endoscope can pass, a guidewire is placed in the distal duodenum or proximal jejunum and left in place as the endoscope is withdrawn. If it cannot pass, a flexible guidewire (0.025 or 0.035") is advanced beyond the obstruction under fluoroscopic guidance. A 7 or 10 Fr orojejunal catheter is then advanced past the obstruction. The linear endoscope is advanced alongside the catheter, and 250cc of contrast mixture is instilled into the small bowel. Under EUS-guidance, the distended small bowel loop is identified from the stomach, and a cautery-enhanced LAMS is deployed. EPASS method uses a double-balloon enteric tube to improve sonographic visualization. An upper endoscope is advanced into the duodenum, followed by a rigid guidewire beyond the target bowel loop. The endoscope is removed, and a double-balloon tube is advanced over the wire. After the balloons are positioned in the duodenum and jejunum, they are filled with contrast to create a stable, distended bowel segment for LAMS placement. Based on the endoscopist’s experience and instrument availability either of these EUS-guided techniques can be used for the successful creation of gastroenterostomy.
Disclosures:
Arjun Chatterjee, MD1, Raj Jessica Thomas, MD2, Zehra Naseem, MD1, Amandeep Singh, MD2, Prabhleen Chahal, MD1. P2170 - Endoscopic Ultrasound-Guided Gastroenterostomy: An Animated Educational Video Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Akron General, Akron, OH
Introduction: Gastric outlet obstruction (GOO) has been traditionally treated surgically or with duodenal stent. Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has recently emerged as an alternative minimally invasive technique for managing benign and malignant GOO. This animated educational video reviews three EUS-GE techniques: direct, EUS-guided balloon-occluded gastrojejunostomy bypass (EPASS), and orojejunal tube-facilitated contrast-enhanced method.
Case Description/Methods: An 82-year-old man with a malignant bladder tumor presented with worsening nausea, vomiting, and abdominal cramping. Computed tomography scan showed duodenal wall thickening causing GOO. Endoscopy revealed severe stenosis of second part of duodenum. Using orojejunal tube-facilitated contrast-enhanced EUS-GE technique, a lumen apposing metal stent (LAMS) was placed to create EUS-GE. (Figure 1). His symptoms resolved completely, and a small bowel follow-through showed GOO resolution and a patent gastro-jejunal stent.
Discussion: Direct EUS-GE method: a linear endoscope is used to identify the jejunal or distal duodenum loop. Under EUS-guidance, a 19-gauge needle is used to instill a 250cc contrast mixture, followed by deploying a cautery-enhanced LAMS. Safety checks ensure proper alignment. Orojejunal tube-facilitated contrast-enhanced technique: standard or therapeutic endoscope is advanced to the obstruction site. If the endoscope can pass, a guidewire is placed in the distal duodenum or proximal jejunum and left in place as the endoscope is withdrawn. If it cannot pass, a flexible guidewire (0.025 or 0.035") is advanced beyond the obstruction under fluoroscopic guidance. A 7 or 10 Fr orojejunal catheter is then advanced past the obstruction. The linear endoscope is advanced alongside the catheter, and 250cc of contrast mixture is instilled into the small bowel. Under EUS-guidance, the distended small bowel loop is identified from the stomach, and a cautery-enhanced LAMS is deployed. EPASS method uses a double-balloon enteric tube to improve sonographic visualization. An upper endoscope is advanced into the duodenum, followed by a rigid guidewire beyond the target bowel loop. The endoscope is removed, and a double-balloon tube is advanced over the wire. After the balloons are positioned in the duodenum and jejunum, they are filled with contrast to create a stable, distended bowel segment for LAMS placement. Based on the endoscopist’s experience and instrument availability either of these EUS-guided techniques can be used for the successful creation of gastroenterostomy.
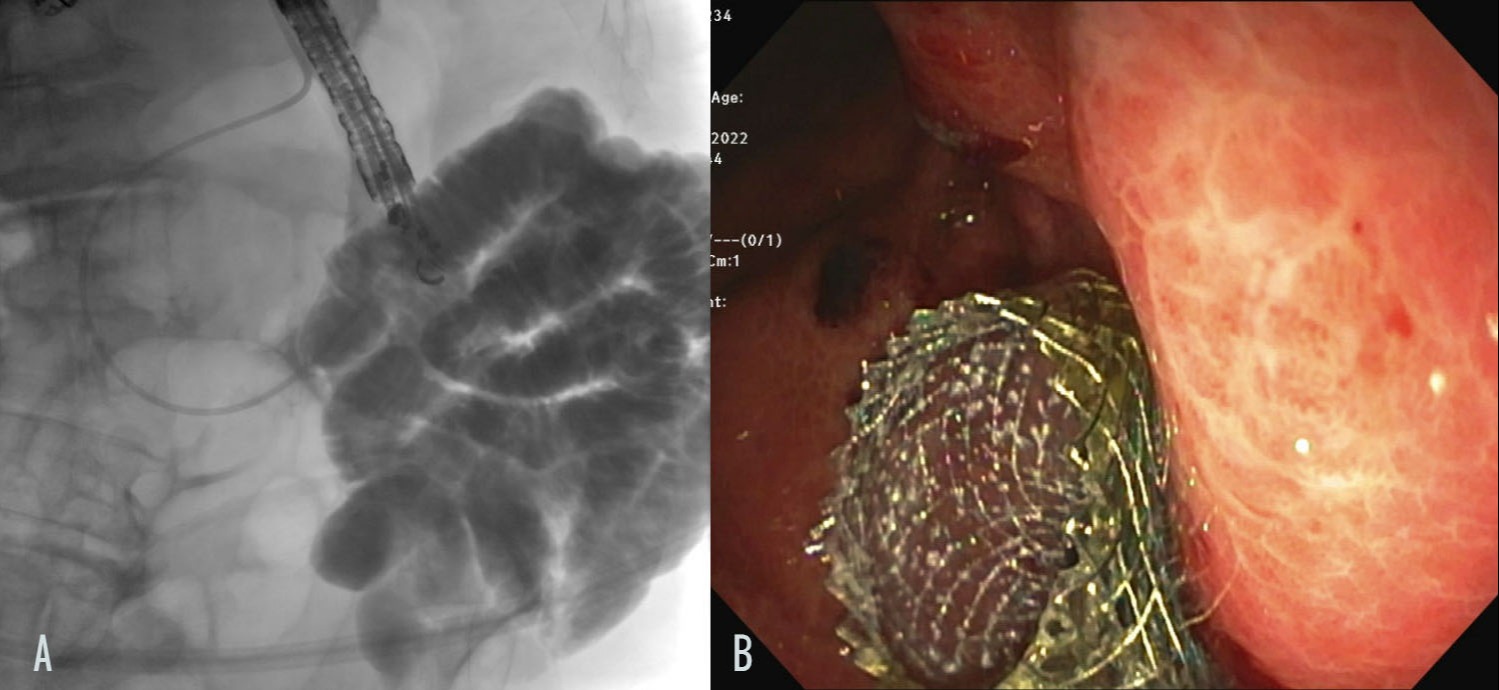
Figure: Figure 1: (A) Naso-biliary drain was placed in the distal duodenum/proximal jejunum over a guidewire and was distended with a mixture of methylene blue and contrast. (B) A 15 x 10 mm LAMS stent was placed through the gastroenterostomy. Methylene blue was seen flowing from the small bowel into the stomach.
Disclosures:
Arjun Chatterjee indicated no relevant financial relationships.
Raj Jessica Thomas indicated no relevant financial relationships.
Zehra Naseem indicated no relevant financial relationships.
Amandeep Singh indicated no relevant financial relationships.
Prabhleen Chahal: Boston Scientific – Advisor or Review Panel Member.
Arjun Chatterjee, MD1, Raj Jessica Thomas, MD2, Zehra Naseem, MD1, Amandeep Singh, MD2, Prabhleen Chahal, MD1. P2170 - Endoscopic Ultrasound-Guided Gastroenterostomy: An Animated Educational Video Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

