Monday Poster Session
Category: Endoscopy Video Forum
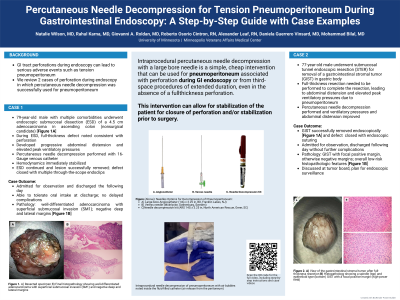
P2182 - Percutaneous Needle Decompression for Tension Pneumoperitoneum During Gastrointestinal Endoscopy: A Step-by-Step Guide With Case Examples
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Natalie Wilson, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Natalie Wilson, MD1, Rahul Karna, MD2, Giovanni Roldan, MD1, Roberto Osorio Cintron, RN3, Alexander Leaf, RN3, Daniela Guerrero Vinsard, MD4, Mohammad Bilal, MD4
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Iatrogenic gastrointestinal tract perforations during endoscopy are rare but can be life-threatening due to tension pneumoperitoneum. Here we describe the technique for percutaneous needle decompression and highlight 2 case examples where it was successfully used for pneumoperitoneum occurring during advanced endoscopic resection.
Case Description/Methods: Case 1: A 79-year-old man with multiple comorbidities was diagnosed with a 4.5 cm adenocarcinoma in the ascending colon. He was referred to colorectal surgery but was determined to be a nonsurgical candidate. After multidisciplinary discussion, the decision was made to pursue endoscopic submucosal dissection (ESD). During ESD, a full thickness defect was noted with visible peritoneal fat. The patient developed progressive abdominal distension and elevated peak ventilatory pressures. The decision was made to perform percutaneous needle decompression. A 16-gauge venous catheter with an attached saline-filled syringe was inserted into the abdomen a few centimeters from the umbilicus and slowly advanced. Immediate release of gas followed (Video). Peak ventilatory pressures and abdominal distention improved. ESD was continued and the lesion was successfully resected. The defect was subsequently closed using through-the-scope endoclips. Case 2: A 77-year-old male underwent submucosal tunnel endoscopic resection for removal of a gastrointestinal stromal tumor (GIST) in the body of the stomach. Due to the nature of the lesion, full thickness resection needed to be performed to complete the resection. This led to progressive abdominal distension and elevated peak ventilatory pressures. Percutaneous needle decompression for pneumoperitoneum was then performed. Ventilatory pressures and abdominal distension improved. Full-thickness resection of the GIST continued and the lesion was successfully resected. Defect closure was performed using endoscopic suturing. Both patients were observed in the hospital overnight and were discharged the following day without further complications.
Discussion: Intraprocedural percutaneous needle decompression is a simple and cheap intervention which can be used for management of pneumoperitoneum and can lead to stabilization of hemodynamic compromise, allowing for endoscopic closure of perforation or as a temporizing measure prior to surgical intervention. Endoscopists should be comfortable performing this potentially lifesaving intervention.
Disclosures:
Natalie Wilson, MD1, Rahul Karna, MD2, Giovanni Roldan, MD1, Roberto Osorio Cintron, RN3, Alexander Leaf, RN3, Daniela Guerrero Vinsard, MD4, Mohammad Bilal, MD4. P2182 - Percutaneous Needle Decompression for Tension Pneumoperitoneum During Gastrointestinal Endoscopy: A Step-by-Step Guide With Case Examples, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Iatrogenic gastrointestinal tract perforations during endoscopy are rare but can be life-threatening due to tension pneumoperitoneum. Here we describe the technique for percutaneous needle decompression and highlight 2 case examples where it was successfully used for pneumoperitoneum occurring during advanced endoscopic resection.
Case Description/Methods: Case 1: A 79-year-old man with multiple comorbidities was diagnosed with a 4.5 cm adenocarcinoma in the ascending colon. He was referred to colorectal surgery but was determined to be a nonsurgical candidate. After multidisciplinary discussion, the decision was made to pursue endoscopic submucosal dissection (ESD). During ESD, a full thickness defect was noted with visible peritoneal fat. The patient developed progressive abdominal distension and elevated peak ventilatory pressures. The decision was made to perform percutaneous needle decompression. A 16-gauge venous catheter with an attached saline-filled syringe was inserted into the abdomen a few centimeters from the umbilicus and slowly advanced. Immediate release of gas followed (Video). Peak ventilatory pressures and abdominal distention improved. ESD was continued and the lesion was successfully resected. The defect was subsequently closed using through-the-scope endoclips. Case 2: A 77-year-old male underwent submucosal tunnel endoscopic resection for removal of a gastrointestinal stromal tumor (GIST) in the body of the stomach. Due to the nature of the lesion, full thickness resection needed to be performed to complete the resection. This led to progressive abdominal distension and elevated peak ventilatory pressures. Percutaneous needle decompression for pneumoperitoneum was then performed. Ventilatory pressures and abdominal distension improved. Full-thickness resection of the GIST continued and the lesion was successfully resected. Defect closure was performed using endoscopic suturing. Both patients were observed in the hospital overnight and were discharged the following day without further complications.
Discussion: Intraprocedural percutaneous needle decompression is a simple and cheap intervention which can be used for management of pneumoperitoneum and can lead to stabilization of hemodynamic compromise, allowing for endoscopic closure of perforation or as a temporizing measure prior to surgical intervention. Endoscopists should be comfortable performing this potentially lifesaving intervention.
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Giovanni Roldan indicated no relevant financial relationships.
Roberto Osorio Cintron indicated no relevant financial relationships.
Alexander Leaf indicated no relevant financial relationships.
Daniela Guerrero Vinsard indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Natalie Wilson, MD1, Rahul Karna, MD2, Giovanni Roldan, MD1, Roberto Osorio Cintron, RN3, Alexander Leaf, RN3, Daniela Guerrero Vinsard, MD4, Mohammad Bilal, MD4. P2182 - Percutaneous Needle Decompression for Tension Pneumoperitoneum During Gastrointestinal Endoscopy: A Step-by-Step Guide With Case Examples, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
