Monday Poster Session
Category: Esophagus
P2183 - Unmet Needs Among Patients with Eosinophilic Esophagitis Despite Biologic Use
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- FE
Flavia Ejzykowicz, PhD
Bristol Myers Squibb
Princeton, NJ
Presenting Author(s)
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, James Siddall, BA3, Chris Higgins, PharmD2, Luc Biedermann, MD4
1University of Michigan, Ann Arbor, MI; 2Bristol Myers Squibb, Princeton, NJ; 3Adelphi Real World, Bollington, England, United Kingdom; 4Universitäts Spital Zürich, Zurich, Zurich, Switzerland
Introduction: Eosinophilic esophagitis (EoE) is a chronic, progressive, type 2 inflammatory disease characterized by symptoms of esophageal dysfunction and eosinophilic inflammation. Recent changes in the EoE treatment landscape include the emergence of biologics and development of other novel therapies; however, it is unknown whether treatment needs have been fully met by these pharmacological advances. This real-world analysis was conducted to explore the unmet need in EoE among patients receiving a biologic as their main treatment in the Adelphi EoE Disease Specific Programme™ (DSP).
Methods: Data were drawn from the DSP, a real-world, cross-sectional survey of physicians and their patients with confirmed diagnosis of EoE in the US, UK, and EU (France, Germany, Italy, Spain) from July through December 2023. Analyses were based on clinical data drawn from medical records, and included treatment type, patient symptoms, and adaptive eating behaviors. Analyses were descriptive with results presented for the subset of patients using biologics, which represents the most advanced pharmacologic treatment available.
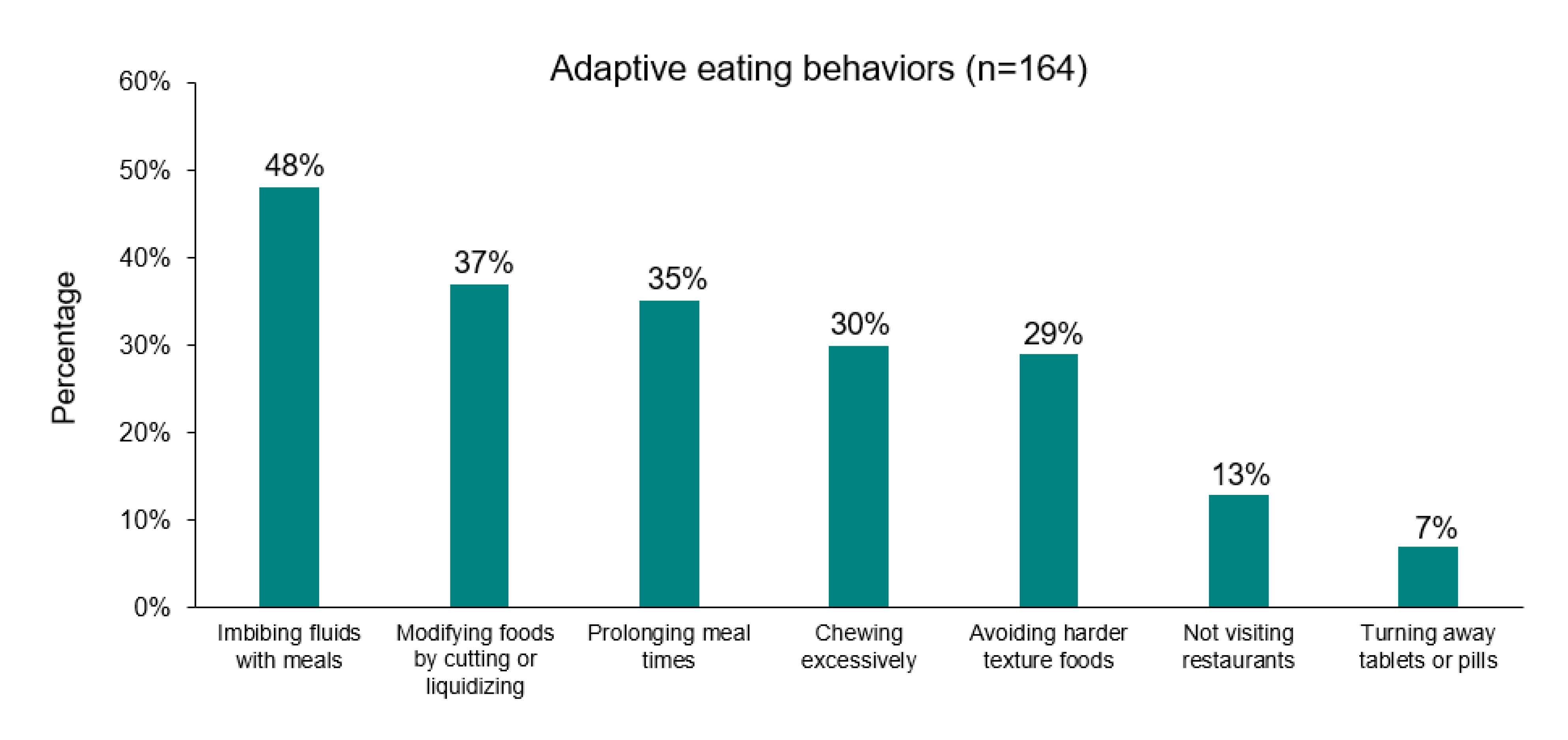
Results: Physicians provided data on 176 patients (31% female; mean age, 35.9 years; 83% White; 70% US based vs 30% Europe based) who received biologics (including anti-interleukin-4 receptor alpha [IL-4Rα] antibody, anti-IL5 antibody, anti-IL13 antibody, anti-thymic stromal lymphopoietin antibody, and anti-Immunoglobulin E antibody) as their main treatment for EoE (Table 1). Although an anti-IL-4Rα antibody is the only approved biologic for EoE, physicians indicated that the current biologic treatment noted was the “main” treatment for EoE. In total, 39% (n=69) of patients had a concurrent diagnosis of asthma. Although physicians felt that most patients (75%) experienced symptomatic relief from their current treatment, they noted that patients had persistent adaptive eating behaviors (Figure 1).
Discussion: Despite experiencing symptomatic improvements following biologic use, most patients with EoE continue to adapt their eating behavior, suggesting an unmet need for optimized symptom control and accurate assessment of symptom resolution with available advanced therapies.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, James Siddall, BA3, Chris Higgins, PharmD2, Luc Biedermann, MD4. P2183 - Unmet Needs Among Patients with Eosinophilic Esophagitis Despite Biologic Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Bristol Myers Squibb, Princeton, NJ; 3Adelphi Real World, Bollington, England, United Kingdom; 4Universitäts Spital Zürich, Zurich, Zurich, Switzerland
Introduction: Eosinophilic esophagitis (EoE) is a chronic, progressive, type 2 inflammatory disease characterized by symptoms of esophageal dysfunction and eosinophilic inflammation. Recent changes in the EoE treatment landscape include the emergence of biologics and development of other novel therapies; however, it is unknown whether treatment needs have been fully met by these pharmacological advances. This real-world analysis was conducted to explore the unmet need in EoE among patients receiving a biologic as their main treatment in the Adelphi EoE Disease Specific Programme™ (DSP).
Methods: Data were drawn from the DSP, a real-world, cross-sectional survey of physicians and their patients with confirmed diagnosis of EoE in the US, UK, and EU (France, Germany, Italy, Spain) from July through December 2023. Analyses were based on clinical data drawn from medical records, and included treatment type, patient symptoms, and adaptive eating behaviors. Analyses were descriptive with results presented for the subset of patients using biologics, which represents the most advanced pharmacologic treatment available.
Results: Physicians provided data on 176 patients (31% female; mean age, 35.9 years; 83% White; 70% US based vs 30% Europe based) who received biologics (including anti-interleukin-4 receptor alpha [IL-4Rα] antibody, anti-IL5 antibody, anti-IL13 antibody, anti-thymic stromal lymphopoietin antibody, and anti-Immunoglobulin E antibody) as their main treatment for EoE (Table 1). Although an anti-IL-4Rα antibody is the only approved biologic for EoE, physicians indicated that the current biologic treatment noted was the “main” treatment for EoE. In total, 39% (n=69) of patients had a concurrent diagnosis of asthma. Although physicians felt that most patients (75%) experienced symptomatic relief from their current treatment, they noted that patients had persistent adaptive eating behaviors (Figure 1).
Discussion: Despite experiencing symptomatic improvements following biologic use, most patients with EoE continue to adapt their eating behavior, suggesting an unmet need for optimized symptom control and accurate assessment of symptom resolution with available advanced therapies.
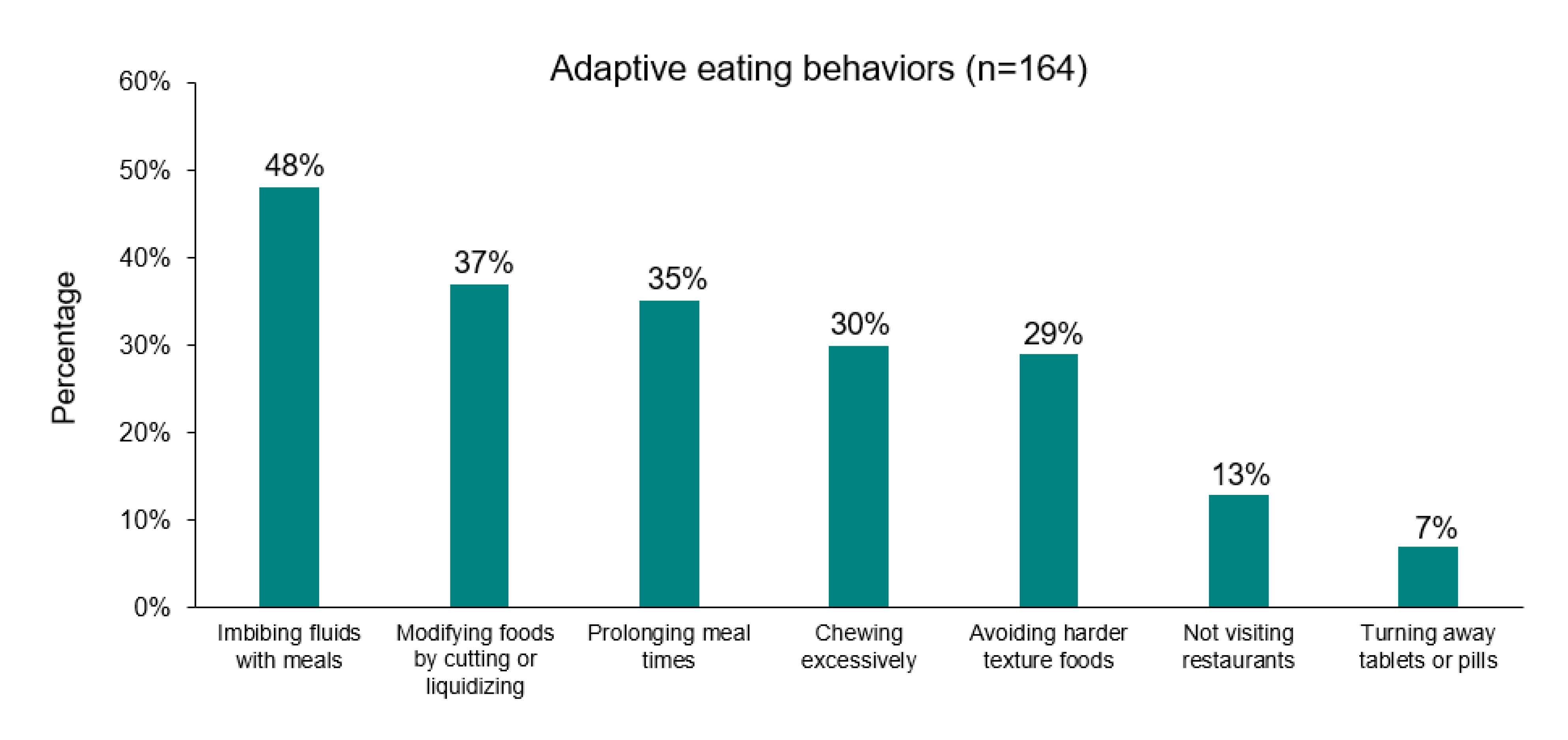
Figure: Figure 1. Adaptive behaviors in post-biologic treatment
Note: The question asked was “Does the patient use any accommodation methods to cope with their symptoms?”
Note: The question asked was “Does the patient use any accommodation methods to cope with their symptoms?”
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang: Bristol Meyers Squibb – Consultant. Sanofi Regeneron – Consultant. Takeda Pharmaceuticals – Consultant.
Flavia Ejzykowicz: Bristol Myers Squibb – Employee, Stock Options.
Carla Zema: Bristol Myers Squibb – Grant/Research Support, Contractor.
Daniel Mascia: Bristol Myers Squibb – Abstract Support.
James Siddall indicated no relevant financial relationships.
Chris Higgins: Bristol Myers Squibb – Employee, Support for the present manuscript and support to attend meetings.
Luc Biedermann: Abbvie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant. Calypso – Advisory Committee/Board Member. Esocap – Advisory Committee/Board Member. Falk – Advisory Committee/Board Member, Consultant. Ferring – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Lilly – Advisory Committee/Board Member. MSD – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Takeda Pharmaceuticals – Advisory Committee/Board Member, Consultant. Vifor – Advisory Committee/Board Member.
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, James Siddall, BA3, Chris Higgins, PharmD2, Luc Biedermann, MD4. P2183 - Unmet Needs Among Patients with Eosinophilic Esophagitis Despite Biologic Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
