Monday Poster Session
Category: Esophagus
P2184 - Clinicians Report Uncertainty Regarding Approaches to Treatment Beyond Proton Pump Inhibitors in Eosinophilic Esophagitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
.jpg)
Joy Chang, MD, MS
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Joy Chang, MD, MS1, Kelcie Brophy, BS2, Kerry Ryan, MA3, Joel H. Rubenstein, MD, MSCI4, Evan S.. Dellon, MD, MPH, FACG5, Lauren P. Wallner, PhD, MPH1, Raymond De Vries, PhD3
1University of Michigan, Ann Arbor, MI; 2Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School, Cincinnati, OH; 3Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School, Ann Arbor, MI; 4Veterans Affairs Center for Clinical Management Research, Ann Arbor VA Medical Center, University of Michigan, Ann Arbor, MI; 5University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
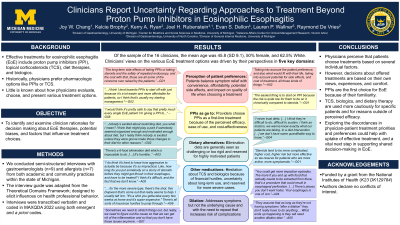
Introduction: Treatments for eosinophilic esophagitis (EoE) include proton pump inhibitors (PPI), topical steroids, diet therapies, and biologics. Physicians historically favor pharmacologic options for EoE, but little is known about how they evaluate, choose, and present various treatments to patients. Our study identifies and examines clinician rationales for decision making about EoE therapies, potential biases, and factors that influence treatment choices.
Methods: We conducted semi-structured interviews with gastroenterologists (n=9) and allergists (n=7) from both academic and community practice settings across the state of Michigan. Our interview guide was developed by adapting classifications from the Theoretical Domains Framework for understanding influences on health professional behavior. Interviews were transcribed verbatim and coded using both emergent and a priori codes.
Results: A total of 16 clinicians were interviewed (45.8 mean age, SD 9.1, 50% female, 62.5% White). Thematic saturation was reached after 16 interviews. Five themes emerged from qualitative analysis: 1) Perception of patient preferences: Belief that patients elect treatments that balance symptom relief with convenience, affordability, potential side effects, and impact on quality of life. 2) PPI as go-to: Clinicians choose PPIs as a first-line treatment for EoE because of its perceived efficacy, ease of use, and cost-effectiveness; 3) Dietary alternatives: elimination diets are generally seen as challenging or too rigid, reserved for highly motivated patients. 4) Other medications: hesitation about steroids and biologics because of financial hurdles, uncertainty about long-term use, and reserved for more severe cases. 5) Dilation: a treatment that addresses symptoms but not the underlying cause and with the need to repeat that increases risk of complications (Table 1).
Discussion: Although clinicians perceive that patients choose treatments based on several individual factors, decisions about offered treatments are based on their own views, experiences, and comfort. PPIs are a common and familiar first choice for EoE, with other pharmacologic and dietary therapies used more cautiously for specific patients and for reasons outside of perceived efficacy. Because effective treatments are available but uptake is poor, exploring discordances in clinician and patient treatment priorities and preferences is a crucial next step in supporting successful shared decision making in EoE.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang, MD, MS1, Kelcie Brophy, BS2, Kerry Ryan, MA3, Joel H. Rubenstein, MD, MSCI4, Evan S.. Dellon, MD, MPH, FACG5, Lauren P. Wallner, PhD, MPH1, Raymond De Vries, PhD3. P2184 - Clinicians Report Uncertainty Regarding Approaches to Treatment Beyond Proton Pump Inhibitors in Eosinophilic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School, Cincinnati, OH; 3Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School, Ann Arbor, MI; 4Veterans Affairs Center for Clinical Management Research, Ann Arbor VA Medical Center, University of Michigan, Ann Arbor, MI; 5University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
Introduction: Treatments for eosinophilic esophagitis (EoE) include proton pump inhibitors (PPI), topical steroids, diet therapies, and biologics. Physicians historically favor pharmacologic options for EoE, but little is known about how they evaluate, choose, and present various treatments to patients. Our study identifies and examines clinician rationales for decision making about EoE therapies, potential biases, and factors that influence treatment choices.
Methods: We conducted semi-structured interviews with gastroenterologists (n=9) and allergists (n=7) from both academic and community practice settings across the state of Michigan. Our interview guide was developed by adapting classifications from the Theoretical Domains Framework for understanding influences on health professional behavior. Interviews were transcribed verbatim and coded using both emergent and a priori codes.
Results: A total of 16 clinicians were interviewed (45.8 mean age, SD 9.1, 50% female, 62.5% White). Thematic saturation was reached after 16 interviews. Five themes emerged from qualitative analysis: 1) Perception of patient preferences: Belief that patients elect treatments that balance symptom relief with convenience, affordability, potential side effects, and impact on quality of life. 2) PPI as go-to: Clinicians choose PPIs as a first-line treatment for EoE because of its perceived efficacy, ease of use, and cost-effectiveness; 3) Dietary alternatives: elimination diets are generally seen as challenging or too rigid, reserved for highly motivated patients. 4) Other medications: hesitation about steroids and biologics because of financial hurdles, uncertainty about long-term use, and reserved for more severe cases. 5) Dilation: a treatment that addresses symptoms but not the underlying cause and with the need to repeat that increases risk of complications (Table 1).
Discussion: Although clinicians perceive that patients choose treatments based on several individual factors, decisions about offered treatments are based on their own views, experiences, and comfort. PPIs are a common and familiar first choice for EoE, with other pharmacologic and dietary therapies used more cautiously for specific patients and for reasons outside of perceived efficacy. Because effective treatments are available but uptake is poor, exploring discordances in clinician and patient treatment priorities and preferences is a crucial next step in supporting successful shared decision making in EoE.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang: Bristol Meyers Squibb – Consultant. Sanofi Regeneron – Consultant. Takeda Pharmaceuticals – Consultant.
Kelcie Brophy indicated no relevant financial relationships.
Kerry Ryan indicated no relevant financial relationships.
Joel Rubenstein indicated no relevant financial relationships.
Evan Dellon: Abbott – Consultant. AbbVie – Consultant. Adare/Ellodi – Consultant, Grant/Research Support. Aimmune – Consultant. Akesobio – Consultant. Alfasigma – Consultant. ALK – Consultant. Allakos – Consultant, Grant/Research Support. Amgen – Consultant. Aqilion – Consultant, Grant/Research Support. Arena/Pfizer – Consultant, Grant/Research Support. Aslan – Consultant. AstraZeneca – Consultant, Grant/Research Support. Avir – Consultant. Biorasi – Consultant. Calypso – Consultant. Celgene/Receptos/BMS – Consultant, Grant/Research Support. Celldex – Consultant. Dr. Falk Pharma – Consultant. Eli Lilly – Consultant. EsoCap – Consultant. Eupraxia – Consultant, Grant/Research Support. Ferring – Consultant, Grant/Research Support. GlaxoSmithKline – Consultant, Grant/Research Support. Gossamer Bio – Consultant. Holoclara – Consultant. Holoclara – Grant/Research Support. Invea – Consultant. Invea – Grant/Research Support. Knightpoint – Consultant. Landos – Consultant. LucidDx – Consultant. Meritage – Grant/Research Support. Miraca – Grant/Research Support. Morphic – Consultant. Nexstone Immunology/Uniquity – Consultant. Nutricia – Consultant, Grant/Research Support. Parexel/Calyx – Consultant. Phathom – Consultant. Regeneron Pharmaceuticals Inc. – Consultant, Grant/Research Support. Revolo – Consultant, Grant/Research Support. Robarts/Alimentiv – Consultant. Salix – Consultant. Sanofi – Consultant. Shire/Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Upstream Bio – Consultant.
Lauren Wallner: Gilead Sciences – Advisor or Review Panel Member.
Raymond De Vries indicated no relevant financial relationships.
Joy Chang, MD, MS1, Kelcie Brophy, BS2, Kerry Ryan, MA3, Joel H. Rubenstein, MD, MSCI4, Evan S.. Dellon, MD, MPH, FACG5, Lauren P. Wallner, PhD, MPH1, Raymond De Vries, PhD3. P2184 - Clinicians Report Uncertainty Regarding Approaches to Treatment Beyond Proton Pump Inhibitors in Eosinophilic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
