Monday Poster Session
Category: Esophagus
P2185 - Assessing the Concordance Between Patients With Eosinophilic Esophagitis and Their Treating Physicians: Evidence From a Real-World Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CH
Chris Higgins, PharmD
Bristol Myers Squibb
Princeton, NJ
Presenting Author(s)
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, Tia Pennant, BSc3, Chris Higgins, PharmD2, Luc Biedermann, MD4
1University of Michigan, Ann Arbor, MI; 2Bristol Myers Squibb, Princeton, NJ; 3Adelphi Real World, Bollington, England, United Kingdom; 4Universitäts Spital Zürich, Zurich, Zurich, Switzerland
Introduction: Eosinophilic esophagitis (EoE) is a chronic disease characterized by esophageal dysfunction and eosinophilic inflammation. A shared understanding of patients’ perceptions and values, along with a comprehensive awareness of the probable prognosis and potential treatment outcomes, is crucial for physicians and patients. Prior research suggests patients prioritize symptom and quality of life (QoL) improvement as treatment outcomes; aligning patient and physician treatment goals can enhance outcomes. We explored patient-physician concordance in EoE treatment.
Methods: Data were drawn from the Adelphi EoE Disease Specific Programme™ (DSP), a real-world, cross-sectional survey with retrospective data collection of physicians and their patients with EoE in EU (France, Germany, Italy, Spain), UK, and US from Jul–Dec 2023. Physicians abstracted clinical data reporting demographics, symptoms, and reasons for choice of treatment for consecutively consulting patients with EoE, and patients reporting their treatment perspectives. Descriptive analyses were performed.
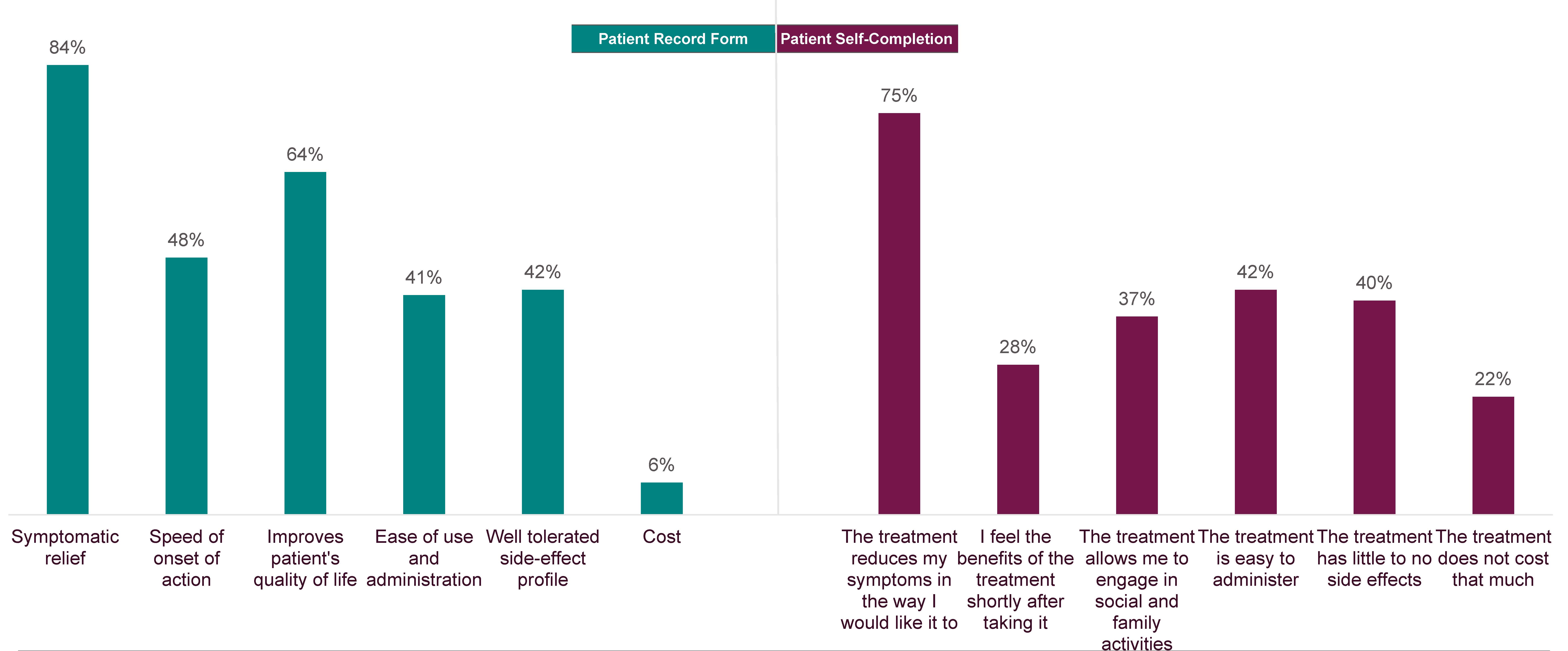
Results: Overall, 190 physicians reported data for 1141 patients, of whom 285 completed a survey. Most patients were male (65%) and White (95%), with a mean (SD) age of 35.8 (12.3) y and mean (SD) duration of current treatment of 1.80 (2.03) y. Prior to diagnosis, the most common symptoms reported were dysphagia (physician: 84% vs patients: 80%), heartburn (60% vs 80%), and food impaction (56% vs 54%); discrepancies were seen in current symptoms: dysphagia (33% vs 43%) and heartburn (36% vs 43%) (Table 1). Physicians reported symptomatic relief (84%), improvements in QoL (64%), and speed of onset (48%) as the most common reasons for selecting current treatment. Patients reported reduction in symptoms (75%), ease of administration (42%), and lack of side effects (40%) as the most common perspectives on treatment (Figure 1). Patients (86% vs 79% of physicians) reported needing additional support such as help with personal care, daily activities, taking medications, or emotional support.
Discussion: Although patient and physician perceptions on reported disease symptoms prior to diagnosis were generally aligned, they were less so on current symptoms. Differences were also seen in physicians’ priorities for choice of treatment and patients’ perspectives on treatment. Further, physicians may underestimate symptom burden and overestimate treatment impact on QoL, leading to unmet needs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, Tia Pennant, BSc3, Chris Higgins, PharmD2, Luc Biedermann, MD4. P2185 - Assessing the Concordance Between Patients With Eosinophilic Esophagitis and Their Treating Physicians: Evidence From a Real-World Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Bristol Myers Squibb, Princeton, NJ; 3Adelphi Real World, Bollington, England, United Kingdom; 4Universitäts Spital Zürich, Zurich, Zurich, Switzerland
Introduction: Eosinophilic esophagitis (EoE) is a chronic disease characterized by esophageal dysfunction and eosinophilic inflammation. A shared understanding of patients’ perceptions and values, along with a comprehensive awareness of the probable prognosis and potential treatment outcomes, is crucial for physicians and patients. Prior research suggests patients prioritize symptom and quality of life (QoL) improvement as treatment outcomes; aligning patient and physician treatment goals can enhance outcomes. We explored patient-physician concordance in EoE treatment.
Methods: Data were drawn from the Adelphi EoE Disease Specific Programme™ (DSP), a real-world, cross-sectional survey with retrospective data collection of physicians and their patients with EoE in EU (France, Germany, Italy, Spain), UK, and US from Jul–Dec 2023. Physicians abstracted clinical data reporting demographics, symptoms, and reasons for choice of treatment for consecutively consulting patients with EoE, and patients reporting their treatment perspectives. Descriptive analyses were performed.
Results: Overall, 190 physicians reported data for 1141 patients, of whom 285 completed a survey. Most patients were male (65%) and White (95%), with a mean (SD) age of 35.8 (12.3) y and mean (SD) duration of current treatment of 1.80 (2.03) y. Prior to diagnosis, the most common symptoms reported were dysphagia (physician: 84% vs patients: 80%), heartburn (60% vs 80%), and food impaction (56% vs 54%); discrepancies were seen in current symptoms: dysphagia (33% vs 43%) and heartburn (36% vs 43%) (Table 1). Physicians reported symptomatic relief (84%), improvements in QoL (64%), and speed of onset (48%) as the most common reasons for selecting current treatment. Patients reported reduction in symptoms (75%), ease of administration (42%), and lack of side effects (40%) as the most common perspectives on treatment (Figure 1). Patients (86% vs 79% of physicians) reported needing additional support such as help with personal care, daily activities, taking medications, or emotional support.
Discussion: Although patient and physician perceptions on reported disease symptoms prior to diagnosis were generally aligned, they were less so on current symptoms. Differences were also seen in physicians’ priorities for choice of treatment and patients’ perspectives on treatment. Further, physicians may underestimate symptom burden and overestimate treatment impact on QoL, leading to unmet needs.
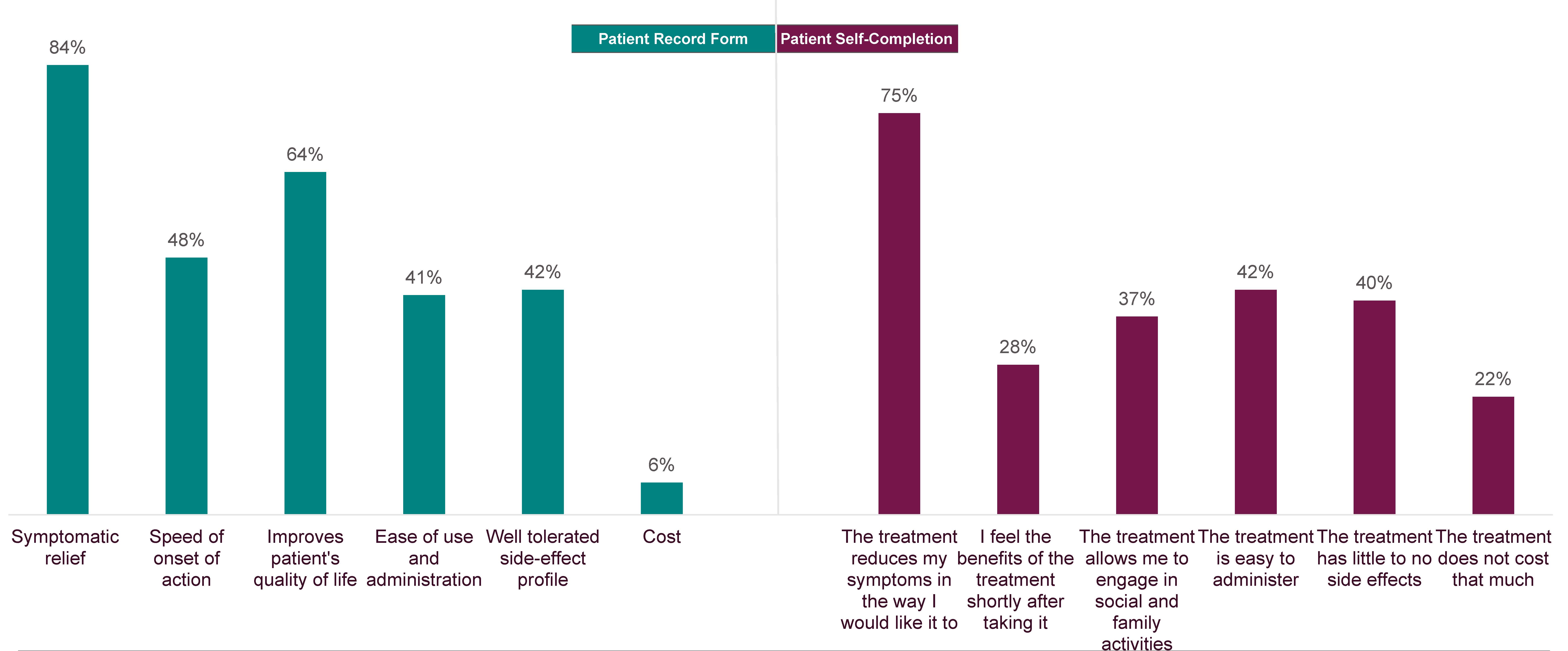
Figure: Figure 1. Physician-reported reasons for choice of treatment (n=240) and patient-reported perspectives on treatment (n=240). Note: not all questions were answered by the physicians and patients
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Chang: Bristol Meyers Squibb – Consultant. Sanofi Regeneron – Consultant. Takeda Pharmaceuticals – Consultant.
Flavia Ejzykowicz: Bristol Myers Squibb – Employee, Stock Options.
Carla Zema: Bristol Myers Squibb – Grant/Research Support, Contractor.
Daniel Mascia: Bristol Myers Squibb – Abstract Support.
Tia Pennant: Bristol Myers Squibb – Abstract Support.
Chris Higgins: Bristol Myers Squibb – Employee, Support for the present manuscript and support to attend meetings.
Luc Biedermann: Abbvie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant. Calypso – Advisory Committee/Board Member. Esocap – Advisory Committee/Board Member. Falk – Advisory Committee/Board Member, Consultant. Ferring – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Lilly – Advisory Committee/Board Member. MSD – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Takeda Pharmaceuticals – Advisory Committee/Board Member, Consultant. Vifor – Advisory Committee/Board Member.
Joy Chang, MD, MS1, Flavia Ejzykowicz, PhD2, Carla Zema, PhD2, Daniel Mascia, BSc3, Tia Pennant, BSc3, Chris Higgins, PharmD2, Luc Biedermann, MD4. P2185 - Assessing the Concordance Between Patients With Eosinophilic Esophagitis and Their Treating Physicians: Evidence From a Real-World Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
