Monday Poster Session
Category: Esophagus
P2187 - Risk of Barrett’s Esophagus in Eosinophilic Esophagitis: A Multi-Center Research Network Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SM
Soban Maan, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Soban Maan, MD1, Rohit Agrawal, MD2, Muhammad Waleed, MD1, Shyam Thakkar, MD1, Shailendra Singh, MD1
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: Data on the risk of Barrett’s esophagus (BE) in eosinophilic esophagitis (EoE) are lacking. We utilized a multi-institutional network to assess BE risk in individuals with EoE.
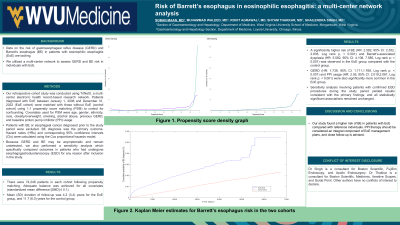
Methods: Our retrospective cohort study was conducted using TriNetX, a multi-center electronic health record-based research network. Patients diagnosed with EoE between January 1, 2006 and December 31, 2022 (EoE cohort) were matched with those without EoE (control cohort) using 1:1 propensity score matching (PSM) to control for confounding. Patients with BE or esophageal cancer diagnosed prior to the study period were excluded. Covariates used for PSM were age, gender, ethnicity, race, obesity/overweight, smoking, alcohol abuse, previous gastroesophageal reflux disease (GERD), and baseline proton pump inhibitor (PPI) usage. BE diagnosis was the primary outcome. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated using the Cox proportional hazards model. Because GERD and BE may be asymptomatic and remain undetected, we performed a sensitivity analysis which specifically compared outcomes in patients who had undergone esophagogastroduodenoscopy (EGD) for any reason after inclusion in the study.
Results: There were 74,248 patients in each cohort following propensity matching. Adequate balance was achieved for all covariates (standardized mean difference [SMD] ≤ 0.1) (Table 1). Mean (SD) duration of follow-up was 4.2 (3.4) years for the EoE group, and 11.7 (6.0) years for the control group. A significantly higher risk of BE (HR: 2.582, 95% CI: 2.352, 2.835, Log rank p, < 0.001) and Barrett’s-associated dysplasia (HR: 5.582, 95% CI: 4.108, 7.585, Log rank p: < 0.001) was observed in the EoE group compared with the control group. GERD (HR: 1.739, 95% CI: 1.711,1.768, Log rank p: < 0.001) and PPI usage (HR: 2.05, 95% CI: 2.019,2.081, Log rank p: < 0.001) were also significantly more common in the EoE group. Sensitivity analysis involving patients with confirmed EGD procedures during the study period yielded results consistent with the primary findings, and all statistically significant associations remained unchanged.
Discussion: Our study found a higher risk of BE in patients with EoE compared with reference individuals. PPI therapy should be considered an integral component of EoE management, and close follow-up is advised.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Soban Maan, MD1, Rohit Agrawal, MD2, Muhammad Waleed, MD1, Shyam Thakkar, MD1, Shailendra Singh, MD1. P2187 - Risk of Barrett’s Esophagus in Eosinophilic Esophagitis: A Multi-Center Research Network Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: Data on the risk of Barrett’s esophagus (BE) in eosinophilic esophagitis (EoE) are lacking. We utilized a multi-institutional network to assess BE risk in individuals with EoE.
Methods: Our retrospective cohort study was conducted using TriNetX, a multi-center electronic health record-based research network. Patients diagnosed with EoE between January 1, 2006 and December 31, 2022 (EoE cohort) were matched with those without EoE (control cohort) using 1:1 propensity score matching (PSM) to control for confounding. Patients with BE or esophageal cancer diagnosed prior to the study period were excluded. Covariates used for PSM were age, gender, ethnicity, race, obesity/overweight, smoking, alcohol abuse, previous gastroesophageal reflux disease (GERD), and baseline proton pump inhibitor (PPI) usage. BE diagnosis was the primary outcome. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated using the Cox proportional hazards model. Because GERD and BE may be asymptomatic and remain undetected, we performed a sensitivity analysis which specifically compared outcomes in patients who had undergone esophagogastroduodenoscopy (EGD) for any reason after inclusion in the study.
Results: There were 74,248 patients in each cohort following propensity matching. Adequate balance was achieved for all covariates (standardized mean difference [SMD] ≤ 0.1) (Table 1). Mean (SD) duration of follow-up was 4.2 (3.4) years for the EoE group, and 11.7 (6.0) years for the control group. A significantly higher risk of BE (HR: 2.582, 95% CI: 2.352, 2.835, Log rank p, < 0.001) and Barrett’s-associated dysplasia (HR: 5.582, 95% CI: 4.108, 7.585, Log rank p: < 0.001) was observed in the EoE group compared with the control group. GERD (HR: 1.739, 95% CI: 1.711,1.768, Log rank p: < 0.001) and PPI usage (HR: 2.05, 95% CI: 2.019,2.081, Log rank p: < 0.001) were also significantly more common in the EoE group. Sensitivity analysis involving patients with confirmed EGD procedures during the study period yielded results consistent with the primary findings, and all statistically significant associations remained unchanged.
Discussion: Our study found a higher risk of BE in patients with EoE compared with reference individuals. PPI therapy should be considered an integral component of EoE management, and close follow-up is advised.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Soban Maan indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Muhammad Waleed indicated no relevant financial relationships.
Shyam Thakkar: Boston Scientific – Consultant. Guide Point – Consultant. Iterative Scopes – Consultant. Medtronic – Consultant. Steris – Consultant.
Shailendra Singh: Apollo Endosurgery – Consultant. Boston Scientific – Consultant. Fujifilm Endoscopy – Consultant.
Soban Maan, MD1, Rohit Agrawal, MD2, Muhammad Waleed, MD1, Shyam Thakkar, MD1, Shailendra Singh, MD1. P2187 - Risk of Barrett’s Esophagus in Eosinophilic Esophagitis: A Multi-Center Research Network Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
