Monday Poster Session
Category: Esophagus
P2188 - Routine Biopsies for Eosinophilic Esophagitis are Unhelpful in Patients With Dysphagia With a Normal-Appearing Esophagus on Endoscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmun Zafar, DO
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ahmun Zafar, DO1, Mako Koseki, MD1, Daniela Jodorkovsky, MD2, Michael S.. Smith, MD, MBA3
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is an increasingly recognized cause of dysphagia. While esophagogastroduodenoscopy (EGD) can identify characteristic features of EoE such as rings, furrows, and exudates, histologic confirmation through biopsies is required for diagnosis. The sensitivity and specificity of EGD for diagnosing EoE in dysphagia patients remain underexplored. Prior EoE research has assessed the diagnostic utility of EGD in the general population, rather than focusing exclusively on patients with dysphagia. This study evaluates whether routine biopsies are necessary for accurate diagnosis in patients with dysphagia when the esophagus appears normal.
Methods: All patients who had proximal and distal esophageal biopsies while undergoing EGD for dysphagia between 2/2018 and 5/2024 at a single high volume esophageal referral center were considered for analysis. Demographic, endoscopic, and histologic data were collected. Patients were categorized into two groups based on visual findings: normal or abnormal (defined as mention of at least one classic EoE feature: edema, rings, exudates, furrows, or stricture). EoE was defined as at least 15 eosinophils/high-power field in either proximal or distal samples.
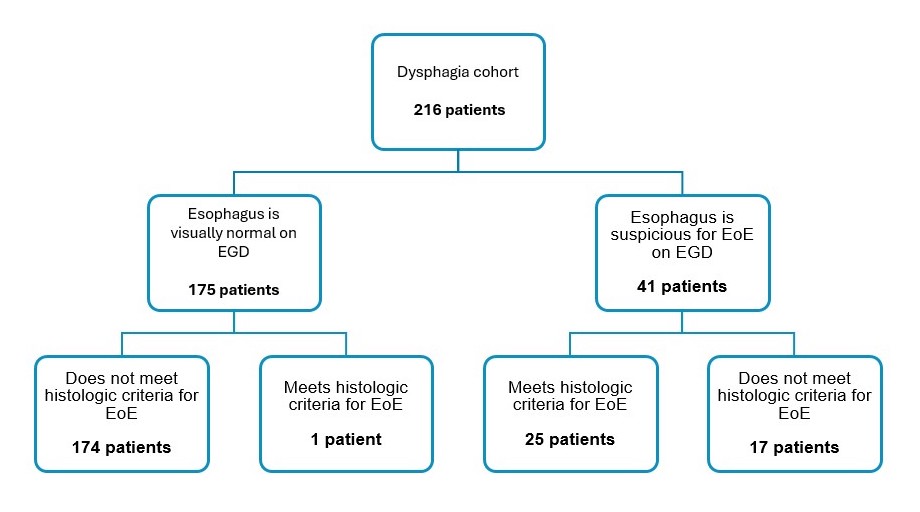
Results: The study included 216 patients with an average age of 51.8 years (58.3% female). Among them, 25 patients (11.6%) met histologic criteria for EoE and were more likely male (p= 0.017) (Table 1). A significantly higher prevalence of EoE was observed in patients with endoscopic findings suggestive of EoE (24/41, 58.5%) compared to those with a normal-appearing esophagus (1/175, 0.6%) (p < 0.001). The positive predictive value (PPV) for classic endoscopic features of EoE was 58.5%, and the negative predictive value (NPV) for normal esophagus on EGD was 99.4%. Sensitivity and specificity for classic endoscopic features of EoE were 96% and 91%, respectively. Of note, the single EoE patient with a normal esophagus was confirmed to have an alternate cause (reflux) of eosinophilia.
Discussion: Among our dysphagia cohort, EoE was significantly more prevalent in patients with abnormal EGD findings. This cohort had a higher sensitivity and NPV for normal EGD compared to existing literature, suggesting a normal EGD is highly effective in excluding EoE when patients have dysphagia. This result should prompt reconsideration of whether to perform routine biopsies in dysphagia patients when the esophagus appears visually normal.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmun Zafar, DO1, Mako Koseki, MD1, Daniela Jodorkovsky, MD2, Michael S.. Smith, MD, MBA3. P2188 - Routine Biopsies for Eosinophilic Esophagitis are Unhelpful in Patients With Dysphagia With a Normal-Appearing Esophagus on Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is an increasingly recognized cause of dysphagia. While esophagogastroduodenoscopy (EGD) can identify characteristic features of EoE such as rings, furrows, and exudates, histologic confirmation through biopsies is required for diagnosis. The sensitivity and specificity of EGD for diagnosing EoE in dysphagia patients remain underexplored. Prior EoE research has assessed the diagnostic utility of EGD in the general population, rather than focusing exclusively on patients with dysphagia. This study evaluates whether routine biopsies are necessary for accurate diagnosis in patients with dysphagia when the esophagus appears normal.
Methods: All patients who had proximal and distal esophageal biopsies while undergoing EGD for dysphagia between 2/2018 and 5/2024 at a single high volume esophageal referral center were considered for analysis. Demographic, endoscopic, and histologic data were collected. Patients were categorized into two groups based on visual findings: normal or abnormal (defined as mention of at least one classic EoE feature: edema, rings, exudates, furrows, or stricture). EoE was defined as at least 15 eosinophils/high-power field in either proximal or distal samples.
Results: The study included 216 patients with an average age of 51.8 years (58.3% female). Among them, 25 patients (11.6%) met histologic criteria for EoE and were more likely male (p= 0.017) (Table 1). A significantly higher prevalence of EoE was observed in patients with endoscopic findings suggestive of EoE (24/41, 58.5%) compared to those with a normal-appearing esophagus (1/175, 0.6%) (p < 0.001). The positive predictive value (PPV) for classic endoscopic features of EoE was 58.5%, and the negative predictive value (NPV) for normal esophagus on EGD was 99.4%. Sensitivity and specificity for classic endoscopic features of EoE were 96% and 91%, respectively. Of note, the single EoE patient with a normal esophagus was confirmed to have an alternate cause (reflux) of eosinophilia.
Discussion: Among our dysphagia cohort, EoE was significantly more prevalent in patients with abnormal EGD findings. This cohort had a higher sensitivity and NPV for normal EGD compared to existing literature, suggesting a normal EGD is highly effective in excluding EoE when patients have dysphagia. This result should prompt reconsideration of whether to perform routine biopsies in dysphagia patients when the esophagus appears visually normal.
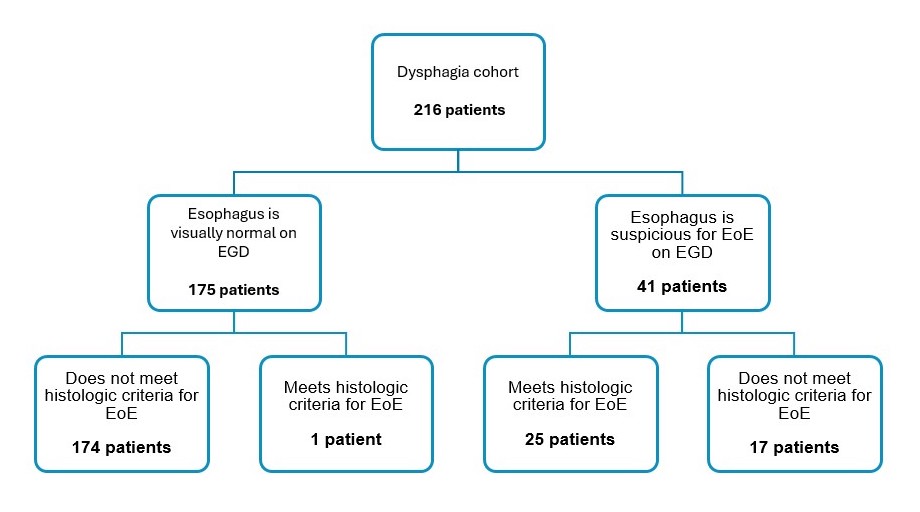
Figure: Prevalence of Eosinophilic Esophagitis (EoE) in Dysphagia Patients Based on Appearance on Esophagogastroduodenoscopy (EGD) and Histologic Findings
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmun Zafar indicated no relevant financial relationships.
Mako Koseki indicated no relevant financial relationships.
Daniela Jodorkovsky: Atmo Biosciences – Consultant.
Michael Smith: Castle Biosciences – Advisory Committee/Board Member, Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Provation Medical – Consultant. Steris Endoscopy – Advisory Committee/Board Member, Consultant.
Ahmun Zafar, DO1, Mako Koseki, MD1, Daniela Jodorkovsky, MD2, Michael S.. Smith, MD, MBA3. P2188 - Routine Biopsies for Eosinophilic Esophagitis are Unhelpful in Patients With Dysphagia With a Normal-Appearing Esophagus on Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
