Monday Poster Session
Category: Esophagus
P2189 - Dysphagia Among Veterans: Are the UES and LES Partners in Crime?
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Christine Son, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Promila Banerjee, MD, FACG1, Christine Son, MD2, Josh Kalapala, BSc1, Binyamin R. Abramowitz, MD3, Jeff Leya, MD4, Bani Chander-Roland, MD, FACG5, Stephen Sontag, MD1
1Edwards Hines Jr. VA Hospital, Maywood, IL; 2Loyola University Medical Center, Maywood, IL; 3SUNY Downstate Health Sciences University, New York, NY; 4Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Dysphagia is most often attributed to esophageal body and lower esophageal sphincter (LES) disorders. Yet, the upper esophageal sphincter (UES) relaxation pattern is not well characterized by the current Chicago classification. Prior studies show incomplete UES relaxation is a rare manometric finding, only associated with achalasia (1), with poor predictive markers of treatment (2,3). This is the first study to assess UES pressure abnormalities primarily or secondary to other LES or esophageal body dysmotility among Veterans over 11 years.
Methods: We conducted a retrospective database study at Hines VA for all patients referred for High-Resolution Manometry from 2013-2024. Mean UES resting and residual pressures were analyzed in these patients diagnosed with body and/or LES dysmotility using Medtronic Manoview ESO 3.3 software. Chi-square tests were performed using SPSS (version 28.0).
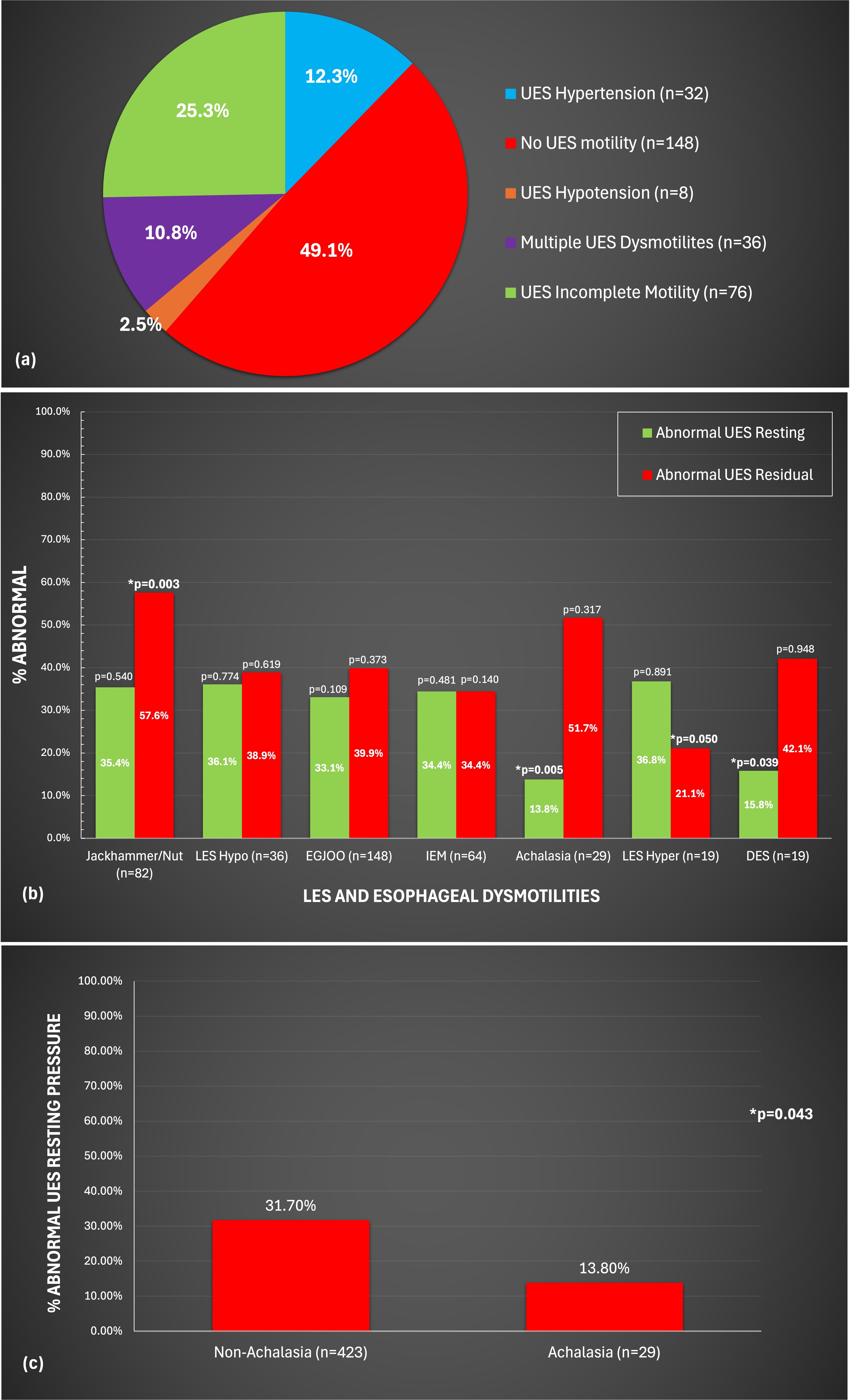
Results: Of 446 Veterans presenting for manometry, 58% had dysphagia, 28% GERD, and 6% for follow-up of prior achalasia. Of those with dysphagia, > 50% were found to have UES abnormalities (Figure 1a).
Of 397 diagnosed with body and LES dysmotility, 46-66% had co-existing UES abnormalities. Abnormal mean UES resting pressures were more frequently found in the non-achalasia vs. achalasia group (p=0.043) (Table 1, Figure 1c). Furthermore, % abnormal mean UES resting pressures among achalasia (p=0.005) and DES (p=0.039) occurred more frequently, whereas % abnormal mean UES residual pressures were more common among Jackhammer (p=0.003) and LES Hypertension (p=0.050) (Figure 1b).
Discussion: UES abnormalities are a frequent finding among Veterans presenting with dysphagia (51%). Up to 66% had co-existing UES dysmotilities in those with body and LES disorders. Abnormal UES residual pressures were more frequently observed in Jackhammer and LES Hypertension. Interestingly, the non-achalasia sub-group, with LES dysfunction, had more frequent UES resting pressure abnormalities as compared to Veterans with achalasia. Further studies are needed to better delineate role of UES abnormalities in esophageal dysmotility.
References
1. DeVault KR. Incomplete UES relaxation: association with achalasia but not other esophageal motility disorders, Dysphagia, 1997 Summer, 12(3), 157–160.
2. Chilukuri, P. et al, Dysphagia, Missouri Med, 2018 May-June, 115(3), 206–210.
3. Mathews SC et al. UES abnormalities are strongly predictive of treatment response in patients with achalasia, World J Clin Cases, 2014 Sep 16, 2(9):448-54.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Promila Banerjee, MD, FACG1, Christine Son, MD2, Josh Kalapala, BSc1, Binyamin R. Abramowitz, MD3, Jeff Leya, MD4, Bani Chander-Roland, MD, FACG5, Stephen Sontag, MD1. P2189 - Dysphagia Among Veterans: Are the UES and LES Partners in Crime?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Edwards Hines Jr. VA Hospital, Maywood, IL; 2Loyola University Medical Center, Maywood, IL; 3SUNY Downstate Health Sciences University, New York, NY; 4Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Dysphagia is most often attributed to esophageal body and lower esophageal sphincter (LES) disorders. Yet, the upper esophageal sphincter (UES) relaxation pattern is not well characterized by the current Chicago classification. Prior studies show incomplete UES relaxation is a rare manometric finding, only associated with achalasia (1), with poor predictive markers of treatment (2,3). This is the first study to assess UES pressure abnormalities primarily or secondary to other LES or esophageal body dysmotility among Veterans over 11 years.
Methods: We conducted a retrospective database study at Hines VA for all patients referred for High-Resolution Manometry from 2013-2024. Mean UES resting and residual pressures were analyzed in these patients diagnosed with body and/or LES dysmotility using Medtronic Manoview ESO 3.3 software. Chi-square tests were performed using SPSS (version 28.0).
Results: Of 446 Veterans presenting for manometry, 58% had dysphagia, 28% GERD, and 6% for follow-up of prior achalasia. Of those with dysphagia, > 50% were found to have UES abnormalities (Figure 1a).
Of 397 diagnosed with body and LES dysmotility, 46-66% had co-existing UES abnormalities. Abnormal mean UES resting pressures were more frequently found in the non-achalasia vs. achalasia group (p=0.043) (Table 1, Figure 1c). Furthermore, % abnormal mean UES resting pressures among achalasia (p=0.005) and DES (p=0.039) occurred more frequently, whereas % abnormal mean UES residual pressures were more common among Jackhammer (p=0.003) and LES Hypertension (p=0.050) (Figure 1b).
Discussion: UES abnormalities are a frequent finding among Veterans presenting with dysphagia (51%). Up to 66% had co-existing UES dysmotilities in those with body and LES disorders. Abnormal UES residual pressures were more frequently observed in Jackhammer and LES Hypertension. Interestingly, the non-achalasia sub-group, with LES dysfunction, had more frequent UES resting pressure abnormalities as compared to Veterans with achalasia. Further studies are needed to better delineate role of UES abnormalities in esophageal dysmotility.
References
1. DeVault KR. Incomplete UES relaxation: association with achalasia but not other esophageal motility disorders, Dysphagia, 1997 Summer, 12(3), 157–160.
2. Chilukuri, P. et al, Dysphagia, Missouri Med, 2018 May-June, 115(3), 206–210.
3. Mathews SC et al. UES abnormalities are strongly predictive of treatment response in patients with achalasia, World J Clin Cases, 2014 Sep 16, 2(9):448-54.
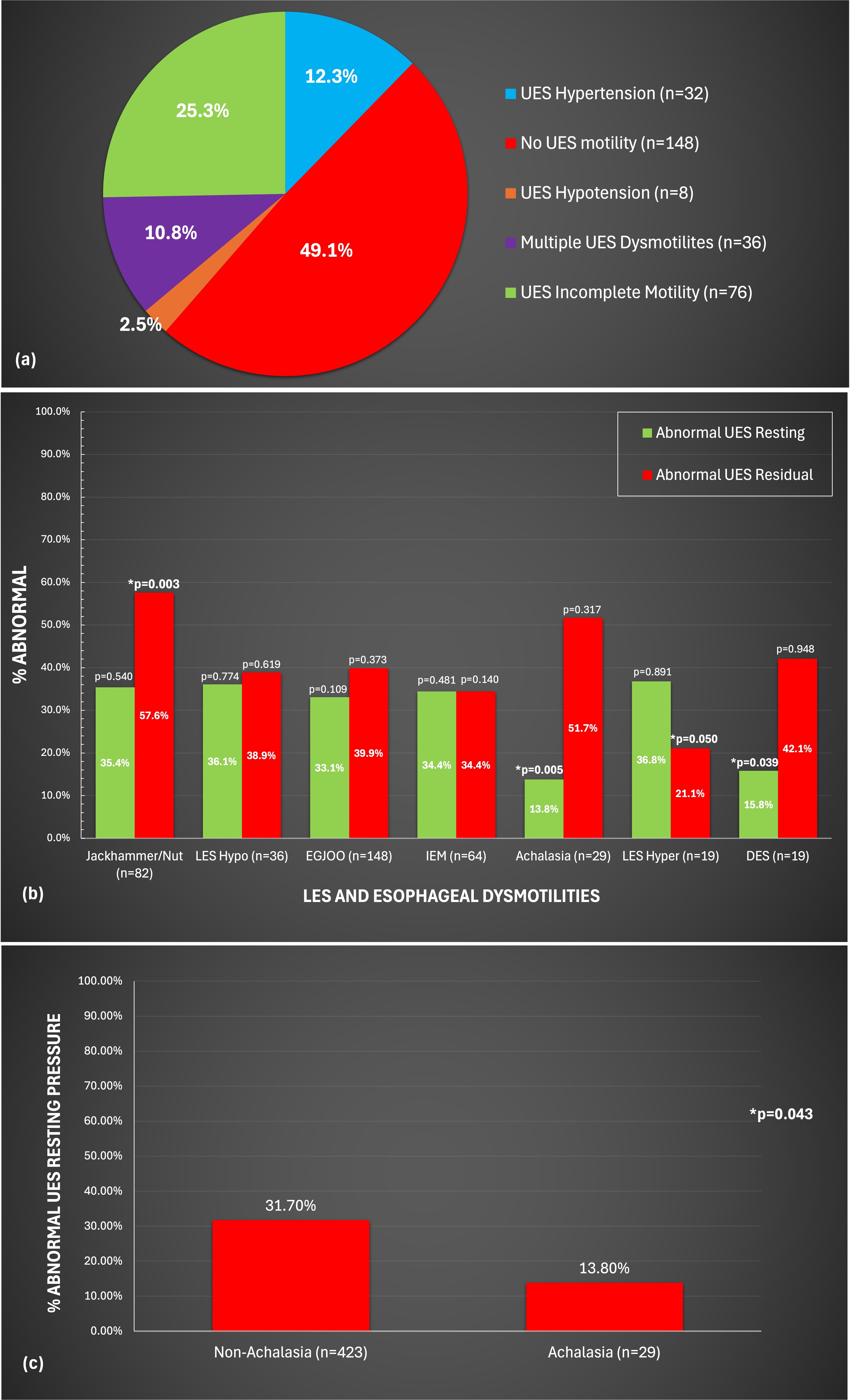
Figure: (a). Distribution of UES Dysmotilites Among Patients Presenting for Manometry. 51% of patients had UES abnormalities.
(b). % Abnormal UES Pressure Values Among LES and Esophageal Body Dysmotilities. Nearly 30-40% had concordant UES abnormal pressures. Achalasia and diffuse esophageal spasm (DES) had significantly increased abnormal UES resting pressure (p=0.005, p=0.039, respectively). Jackhammer nutcracker esophagus and lower esophageal sphincter (LES) hypertension had significantly increased abnormal UES residual pressure (p=0.003, p=0.050, respectively).
(c). % Abnormal UES Resting Values Among Achalasia and Non-Achalasia Patients. Non-achalasia patients had more abnormal UES resting pressures compared to achalasia patients with statistical significance (p=0.043).
(b). % Abnormal UES Pressure Values Among LES and Esophageal Body Dysmotilities. Nearly 30-40% had concordant UES abnormal pressures. Achalasia and diffuse esophageal spasm (DES) had significantly increased abnormal UES resting pressure (p=0.005, p=0.039, respectively). Jackhammer nutcracker esophagus and lower esophageal sphincter (LES) hypertension had significantly increased abnormal UES residual pressure (p=0.003, p=0.050, respectively).
(c). % Abnormal UES Resting Values Among Achalasia and Non-Achalasia Patients. Non-achalasia patients had more abnormal UES resting pressures compared to achalasia patients with statistical significance (p=0.043).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Promila Banerjee indicated no relevant financial relationships.
Christine Son indicated no relevant financial relationships.
Josh Kalapala indicated no relevant financial relationships.
Binyamin Abramowitz indicated no relevant financial relationships.
Jeff Leya indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Stephen Sontag indicated no relevant financial relationships.
Promila Banerjee, MD, FACG1, Christine Son, MD2, Josh Kalapala, BSc1, Binyamin R. Abramowitz, MD3, Jeff Leya, MD4, Bani Chander-Roland, MD, FACG5, Stephen Sontag, MD1. P2189 - Dysphagia Among Veterans: Are the UES and LES Partners in Crime?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
