Monday Poster Session
Category: Esophagus
P2195 - Risk Factors for Esophageal Variceal Ligation Ulcer Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sheema Rehman, DO
Henry Ford Health
Detroit, MI
Presenting Author(s)
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Renieh Nabaty, MD3, Abdulmalik Saleem, MD1, Anas Kutait, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Hospital, Detroit, MI
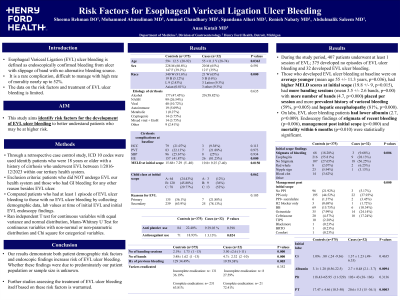
Introduction: Esophageal Variceal Ligation (EVL) ulcer bleeding is defined as endoscopically confirmed bleeding from a post banding ulcer with no alternative bleeding source. EVL ulcer bleeding is a rare complication, difficult to manage and has a high rate of mortality. The data on the risk factors and treatment of EVL ulcer bleeding is limited. This study aims to identify risk factors for the development of EVL ulcer bleeding to better understand patients who may be at higher risk.
Methods: Through a retrospective case control study, ICD 10 codes were used to identify patients who were 18 years or older with a history of cirrhosis who underwent EVL between 1/2016-12/2023 within our tertiary health system. We excluded patients who did not undergo EVL in our health system and those who had GI bleeding for any other reason besides EVL ulcer. We compared patients who had at least 1 episode of EVL ulcer bleeding as defined above to those with no episode of EVL ulcer bleeding by collecting demographic data, lab values at time of initial EVL and initial EVL endoscopy findings. We ran independent T test for continuous variables with equal variance and normal distribution, Mann-Whitney U Test for continuous variables with non-normal or non-parametric distribution and Chi square test for categorial variables.
Results: In this time, 407 patients underwent at least 1 session of EVL in our health system and of these patients, 375 had no episodes of EVL ulcer bleeding and 32 had EVL ulcer bleeding. Those who developed EVL ulcer bleeding at baseline were on average younger (mean age 55 +/- 11.3 years, p=0.036), had higher MELD scores at initial scope (19.8 +/- 9, p=0.015), had more banding sessions (mean 3.5 +/- 2.6 bands, p=0.000) with more number of bands (4.7, p=0.000) placed per session, had a history of variceal bleeding (59%, p=0.005) and hepatic encephalopathy (81%, p=0.000). On labs, EVL ulcer bleeding patients had lower albumin (2.7, p=0.009). Endoscopy findings of stigmata of recent bleeding (p=0.006), management post initial scope (p=0.000) and mortality within 6 months (p=0.010) were statistically significant between the two groups.
Discussion: Our results demonstrate both the presence of patient specific demographic risk factors and endoscopic findings that increase risk of EVL ulcer bleeding. Whether this was due to predominately our patient population or sample size is unknown. Further studies assessing the treatment of EVL ulcer bleeding itself based on these risk factors is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Renieh Nabaty, MD3, Abdulmalik Saleem, MD1, Anas Kutait, MD1. P2195 - Risk Factors for Esophageal Variceal Ligation Ulcer Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Esophageal Variceal Ligation (EVL) ulcer bleeding is defined as endoscopically confirmed bleeding from a post banding ulcer with no alternative bleeding source. EVL ulcer bleeding is a rare complication, difficult to manage and has a high rate of mortality. The data on the risk factors and treatment of EVL ulcer bleeding is limited. This study aims to identify risk factors for the development of EVL ulcer bleeding to better understand patients who may be at higher risk.
Methods: Through a retrospective case control study, ICD 10 codes were used to identify patients who were 18 years or older with a history of cirrhosis who underwent EVL between 1/2016-12/2023 within our tertiary health system. We excluded patients who did not undergo EVL in our health system and those who had GI bleeding for any other reason besides EVL ulcer. We compared patients who had at least 1 episode of EVL ulcer bleeding as defined above to those with no episode of EVL ulcer bleeding by collecting demographic data, lab values at time of initial EVL and initial EVL endoscopy findings. We ran independent T test for continuous variables with equal variance and normal distribution, Mann-Whitney U Test for continuous variables with non-normal or non-parametric distribution and Chi square test for categorial variables.
Results: In this time, 407 patients underwent at least 1 session of EVL in our health system and of these patients, 375 had no episodes of EVL ulcer bleeding and 32 had EVL ulcer bleeding. Those who developed EVL ulcer bleeding at baseline were on average younger (mean age 55 +/- 11.3 years, p=0.036), had higher MELD scores at initial scope (19.8 +/- 9, p=0.015), had more banding sessions (mean 3.5 +/- 2.6 bands, p=0.000) with more number of bands (4.7, p=0.000) placed per session, had a history of variceal bleeding (59%, p=0.005) and hepatic encephalopathy (81%, p=0.000). On labs, EVL ulcer bleeding patients had lower albumin (2.7, p=0.009). Endoscopy findings of stigmata of recent bleeding (p=0.006), management post initial scope (p=0.000) and mortality within 6 months (p=0.010) were statistically significant between the two groups.
Discussion: Our results demonstrate both the presence of patient specific demographic risk factors and endoscopic findings that increase risk of EVL ulcer bleeding. Whether this was due to predominately our patient population or sample size is unknown. Further studies assessing the treatment of EVL ulcer bleeding itself based on these risk factors is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheema Rehman indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Spandana Alluri indicated no relevant financial relationships.
Renieh Nabaty indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Anas Kutait indicated no relevant financial relationships.
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Renieh Nabaty, MD3, Abdulmalik Saleem, MD1, Anas Kutait, MD1. P2195 - Risk Factors for Esophageal Variceal Ligation Ulcer Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

