Monday Poster Session
Category: Esophagus
P2196 - Esophageal Variceal Ligation Ulcer Bleeding: Outcomes of Different Modalities Used for Treatment
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sheema Rehman, DO
Henry Ford Health
Detroit, MI
Presenting Author(s)
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Abdulmalik Saleem, MD1, Renieh Nabaty, MD3, Anas Kutait, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Hospital, Detroit, MI
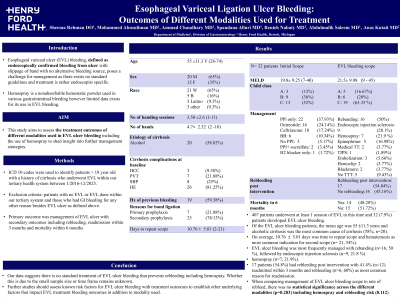
Introduction: Esophageal Variceal Ligation (EVL) ulcer bleeding, defined as endoscopically confirmed bleeding from an ulcer due to slippage of a band with no alternative bleeding source, poses a challenge as there exists no standardized guidelines for treatment. Hemospray is a nonabsorbable hemostatic powder used for various gastrointestinal bleeding, however limited data exists for its use in EVL bleeding. This study aims to assess the treatment outcomes of different modalities used in EVL ulcer bleeding including the use of hemospray to shed insight into management strategies.
Methods: We used ICD 10 codes to identify patients over the age of 18 with a history of cirrhosis who underwent EVL within our tertiary health system between 1/2016-12/2023. We excluded patients who did not have any EVL and those who had GI bleeding for any other reason besides EVL ulcer as defined above. Primary outcome was management of EVL ulcer and secondary outcomes were rebleeding, readmission within 3 months and mortality within 6 months.
Results: 407 patients underwent at least 1 session of EVL in this time and of these, 32 (7.9%) developed EVL ulcer bleeding. Of the EVL ulcer bleeding patients, the mean age was 55 ±11.3 years and alcoholic cirrhosis was the most common cause of cirrhosis (59%, n=19). Mean MELD at initial EVL scope was (19.8± 9.25) compared to MELD at EVL ulcer bleeding scope (21.5± 9.98). On average, 10.76 ±5.01 days was time to repeat scope and hematemesis was most common indication for second scope (n= 21,54%). EVL ulcer bleeding was most frequently managed with rebanding (n=16, 50%), followed by endoscopic injection sclerosis (n=9, 28%) and hemospray (n=7, 22%). 17 patients (53%) had rebleeding post intervention, 12 were (38%) readmitted within 3 months and of these 6 (50%) had rebleeding as the most common reason for readmission.14 (44%) of EVL ulcer bleeding patients died within 6 months. When comparing management of EVL ulcer bleeding scope to rate of rebleed, no statistical significance across the different modalities (p=0.283) including hemospray and rebleeding risk (p=0.112).
Discussion: Our data suggests there is no standard treatment of EVL ulcer bleeding that prevents rebleeding including hemospray. Whether this is due to the small sample size or time frame remains unknown. Further studies should assess known risk factors for EVL ulcer bleeding with treatment outcomes to establish other underlying factors that impact EVL treatment bleeding outcomes in addition to modality used.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Abdulmalik Saleem, MD1, Renieh Nabaty, MD3, Anas Kutait, MD1. P2196 - Esophageal Variceal Ligation Ulcer Bleeding: Outcomes of Different Modalities Used for Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Esophageal Variceal Ligation (EVL) ulcer bleeding, defined as endoscopically confirmed bleeding from an ulcer due to slippage of a band with no alternative bleeding source, poses a challenge as there exists no standardized guidelines for treatment. Hemospray is a nonabsorbable hemostatic powder used for various gastrointestinal bleeding, however limited data exists for its use in EVL bleeding. This study aims to assess the treatment outcomes of different modalities used in EVL ulcer bleeding including the use of hemospray to shed insight into management strategies.
Methods: We used ICD 10 codes to identify patients over the age of 18 with a history of cirrhosis who underwent EVL within our tertiary health system between 1/2016-12/2023. We excluded patients who did not have any EVL and those who had GI bleeding for any other reason besides EVL ulcer as defined above. Primary outcome was management of EVL ulcer and secondary outcomes were rebleeding, readmission within 3 months and mortality within 6 months.
Results: 407 patients underwent at least 1 session of EVL in this time and of these, 32 (7.9%) developed EVL ulcer bleeding. Of the EVL ulcer bleeding patients, the mean age was 55 ±11.3 years and alcoholic cirrhosis was the most common cause of cirrhosis (59%, n=19). Mean MELD at initial EVL scope was (19.8± 9.25) compared to MELD at EVL ulcer bleeding scope (21.5± 9.98). On average, 10.76 ±5.01 days was time to repeat scope and hematemesis was most common indication for second scope (n= 21,54%). EVL ulcer bleeding was most frequently managed with rebanding (n=16, 50%), followed by endoscopic injection sclerosis (n=9, 28%) and hemospray (n=7, 22%). 17 patients (53%) had rebleeding post intervention, 12 were (38%) readmitted within 3 months and of these 6 (50%) had rebleeding as the most common reason for readmission.14 (44%) of EVL ulcer bleeding patients died within 6 months. When comparing management of EVL ulcer bleeding scope to rate of rebleed, no statistical significance across the different modalities (p=0.283) including hemospray and rebleeding risk (p=0.112).
Discussion: Our data suggests there is no standard treatment of EVL ulcer bleeding that prevents rebleeding including hemospray. Whether this is due to the small sample size or time frame remains unknown. Further studies should assess known risk factors for EVL ulcer bleeding with treatment outcomes to establish other underlying factors that impact EVL treatment bleeding outcomes in addition to modality used.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheema Rehman indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Spandana Alluri indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Renieh Nabaty indicated no relevant financial relationships.
Anas Kutait indicated no relevant financial relationships.
Sheema Rehman, DO1, Mohammed Abusuliman, MD1, Ammad Javaid. Chaudhary, MD1, Spandana Alluri, MS, MD2, Abdulmalik Saleem, MD1, Renieh Nabaty, MD3, Anas Kutait, MD1. P2196 - Esophageal Variceal Ligation Ulcer Bleeding: Outcomes of Different Modalities Used for Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
