Monday Poster Session
Category: Esophagus
P2206 - Outcome of Radiation-Related Esophageal Stricture From Endoscopic Dilation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Elliot Axel Baerman, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Elliot Axel. Baerman, MD1, Carolina Colli Cruz, MD2, Samuel C. Black, MD1, Saivaroon Gajagowni, MD1, Brian Weston, MD2, Yinghong Wang, MD, PhD3
1Baylor College of Medicine, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3University of Texas MD Anderson Cancer Center, Houston, TX
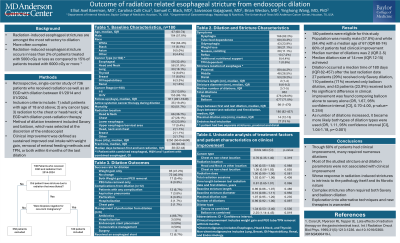
Introduction: Esophageal strictures present a significant challenge, particularly in cases of radiation-induced strictures. Esophageal dilation is a commonly used intervention aimed at improving swallowing function and nutritional status. However, radiation-induced strictures are amongst the most refractory to dilation. Understanding the success and limitations of this procedure is crucial for optimizing patient outcomes in the cancer population.
Methods: This was a single-center retrospective chart review of 736 patients who received radiation as well as an EGD between 2014 and 2024. Patients without a radiation-induced stricture that was dilated were excluded. All continuous data are summarized as medians with interquartile ranges (IQR). Independent t-test was used for comparison among different groups.
Results: 192 were eligible for this study. Our population was mostly male (58%) with a median age of 66 (IQR 67-74). The leading cancer diagnosis were esophageal (37%), head and neck (30.2%), and lung (17.1%). Radiation targets were head and neck (50.5%), lung (45.3%), both (1.6%), or other (1.6%). Patients were receiving active chemotherapy in 9.9% of cases. Mortality by the end of the study period was 51%. The median radiation dose was 5040 cGy (IQR 5040-6600) in a median of 28 fractions (IQR 26-33). Common indications for dilation were dysphagia (91.1%), weight loss (21.9%), and tube feed dependency (17.2%). Strictures were most often dilated 2 to 4 times (39.6%) to a median dilation size of 14 mm (IQR 12-15). Of note, 18.2% of patients needed 8 or more dilations. Dilation was associated with weight gain in 46.4% of patients, PEG tube removal in 3.1%, both forms of improvement in 9.9%, and no change in 40.6%. Complications included perforation (3.6%), aspiration pneumonia (3.6%), chest pain (0.5%), and hospitalization (0.5%). No significant differences were found in maximum dilation size, number of dilations, initial luminal diameter of the stricture, and initial length of the stricture between those who had clinical improvement as compared to those who did not.
Discussion: Our study reported 59.4% clinical improvement from esophageal dilation for radiation-induced strictures with nearly 20% of patients needing 8 or more dilations. The stricture dilation parameters did not appear to affect the success rate. This is the largest known single study of esophageal dilation for radiation-induced strictures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elliot Axel. Baerman, MD1, Carolina Colli Cruz, MD2, Samuel C. Black, MD1, Saivaroon Gajagowni, MD1, Brian Weston, MD2, Yinghong Wang, MD, PhD3. P2206 - Outcome of Radiation-Related Esophageal Stricture From Endoscopic Dilation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Esophageal strictures present a significant challenge, particularly in cases of radiation-induced strictures. Esophageal dilation is a commonly used intervention aimed at improving swallowing function and nutritional status. However, radiation-induced strictures are amongst the most refractory to dilation. Understanding the success and limitations of this procedure is crucial for optimizing patient outcomes in the cancer population.
Methods: This was a single-center retrospective chart review of 736 patients who received radiation as well as an EGD between 2014 and 2024. Patients without a radiation-induced stricture that was dilated were excluded. All continuous data are summarized as medians with interquartile ranges (IQR). Independent t-test was used for comparison among different groups.
Results: 192 were eligible for this study. Our population was mostly male (58%) with a median age of 66 (IQR 67-74). The leading cancer diagnosis were esophageal (37%), head and neck (30.2%), and lung (17.1%). Radiation targets were head and neck (50.5%), lung (45.3%), both (1.6%), or other (1.6%). Patients were receiving active chemotherapy in 9.9% of cases. Mortality by the end of the study period was 51%. The median radiation dose was 5040 cGy (IQR 5040-6600) in a median of 28 fractions (IQR 26-33). Common indications for dilation were dysphagia (91.1%), weight loss (21.9%), and tube feed dependency (17.2%). Strictures were most often dilated 2 to 4 times (39.6%) to a median dilation size of 14 mm (IQR 12-15). Of note, 18.2% of patients needed 8 or more dilations. Dilation was associated with weight gain in 46.4% of patients, PEG tube removal in 3.1%, both forms of improvement in 9.9%, and no change in 40.6%. Complications included perforation (3.6%), aspiration pneumonia (3.6%), chest pain (0.5%), and hospitalization (0.5%). No significant differences were found in maximum dilation size, number of dilations, initial luminal diameter of the stricture, and initial length of the stricture between those who had clinical improvement as compared to those who did not.
Discussion: Our study reported 59.4% clinical improvement from esophageal dilation for radiation-induced strictures with nearly 20% of patients needing 8 or more dilations. The stricture dilation parameters did not appear to affect the success rate. This is the largest known single study of esophageal dilation for radiation-induced strictures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elliot Baerman indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Samuel Black indicated no relevant financial relationships.
Saivaroon Gajagowni indicated no relevant financial relationships.
Brian Weston indicated no relevant financial relationships.
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Elliot Axel. Baerman, MD1, Carolina Colli Cruz, MD2, Samuel C. Black, MD1, Saivaroon Gajagowni, MD1, Brian Weston, MD2, Yinghong Wang, MD, PhD3. P2206 - Outcome of Radiation-Related Esophageal Stricture From Endoscopic Dilation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
