Monday Poster Session
Category: Esophagus
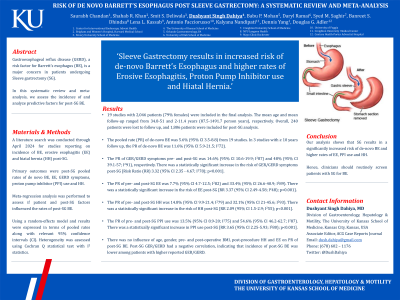
P2216 - Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dushyant S. Dahiya, MD
The University of Kansas School of Medicine
Kansas City, KS
Presenting Author(s)
Saurabh Chandan, MD1, Shahab Khan, MBBS2, Smit Deliwala, MD3, Dushyant S. Dahiya, MD4, Babu Mohan, MD5, Daryl Ramai, MD6, Syed Saghir, MD1, Banreet Dhindsa, MD7, Lena Kassab, MD8, Antonio Facciorusso, MD, PhD9, Kalyana Nandipati, MD10, Dennis Yang, MD11, Douglas Adler, MD12
1CHI Health Creighton University Medical Center, Omaha, NE; 2Brigham and Women's Hospital, Boston, MA; 3Emory University, Atlanta, GA; 4The University of Kansas School of Medicine, Kansas City, KS; 5Orlando Gastroenterology PA, Orlando, FL; 6University of Utah School of Medicine, Salt Lake City, UT; 7NYU Grossman School of Medicine, New York, NY; 8Mayo Clinic, Rochester, MN; 9University of Foggia, Foggia, Puglia, Italy; 10Creighton University School of Medicine, Omaha, NE; 11AdventHealth, Orlando, FL; 12Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Gastroesophageal reflux disease (GERD), a risk factor for Barrett’s esophagus (BE), is a major concern in patients undergoing Sleeve gastrectomy (SG). In this meta-analysis, we assess the incidence of and analyze predictive factors for post-SG BE.
Methods: A literature search was conducted through April 2024 for studies reporting on incidence of BE, erosive esophagitis (EE) and hiatal hernia (HH) post-SG. Primary outcomes were post-SG pooled rates of de novo BE, EE, GERD symptoms, proton pump inhibitor (PPI) use and HH. Meta-regression analysis was performed to assess if patient and post-SG factors influenced the rates of post-SG BE.
Results: 19 studies with 2046 patients (79% females) were included in the final analysis. The mean age and mean follow-up ranged from 34.8-51 and 2-11.4 years (87.5-1491.7 person years), respectively. Overall, 240 patients were lost to follow up, and 1806 patients were included for post-SG analysis.
The pooled rate (PR) of de novo BE was 5.6% (95% CI 3.5-8.8) from 19 studies. In 3 studies with ≥ 10 years follow up, the PR of de novo BE was 11.6% (95% CI 5.9-21.5; I272).
The PR of GER/GERD symptoms pre- and post-SG was 14.6% (95% CI 10.6-19.9; I287) and 48% (95% CI 39.1-57; I291), respectively. There was a statistically significant increase in the risk of GER/GERD symptoms post-SG, Risk Ratio (RR) 3.32 (95% CI 2.35 - 4.67; I2 78); p< 0.001.
The PR of pre- and post-SG EE was 7.7% (95% CI 4.7-12.5; I282) and 33.4% (95% CI 26.6-40.9; I289). There was a statistically significant increase in the risk of EE post-SG, RR 3.37 (95% CI 2.49-4.58; I248); p< 0.001.
The PR of pre- and post-SG HH was 14.8% (95% CI 9.9-21.4; I279) and 32.1% (95% CI 21-45.6; I293). There was a statistically significant increase in the risk of HH post-SG, RR 2.09 (95% CI 1.5-2.9; I2 55); p< 0.001.
The PR of pre- and post-SG PPI use was 13.5% (95% CI 8.9-20; I275) and 54.6% (95% CI 46.2-62.7; I287). There was a statistically significant increase in PPI use post-SG, RR 3.65 (95% CI 2.25-5.93; I2 80); p< 0.001.
Based on meta-regression analysis, there was no influence of age, gender, pre- and post-operative BMI, post-procedure HH and EE on PR of post-SG BE. Post-SG GER/GERD had a negative correlation, indicating that incidence of post-SG BE was lower among patients with higher reported GER/GERD.
Discussion: Our analysis shows that SG results in a significantly increased risk of de novo BE and higher rates of EE, PPI use and HH. Hence, clinicians should routinely screen patients with SG for BE.
Disclosures:
Saurabh Chandan, MD1, Shahab Khan, MBBS2, Smit Deliwala, MD3, Dushyant S. Dahiya, MD4, Babu Mohan, MD5, Daryl Ramai, MD6, Syed Saghir, MD1, Banreet Dhindsa, MD7, Lena Kassab, MD8, Antonio Facciorusso, MD, PhD9, Kalyana Nandipati, MD10, Dennis Yang, MD11, Douglas Adler, MD12. P2216 - Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Omaha, NE; 2Brigham and Women's Hospital, Boston, MA; 3Emory University, Atlanta, GA; 4The University of Kansas School of Medicine, Kansas City, KS; 5Orlando Gastroenterology PA, Orlando, FL; 6University of Utah School of Medicine, Salt Lake City, UT; 7NYU Grossman School of Medicine, New York, NY; 8Mayo Clinic, Rochester, MN; 9University of Foggia, Foggia, Puglia, Italy; 10Creighton University School of Medicine, Omaha, NE; 11AdventHealth, Orlando, FL; 12Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Gastroesophageal reflux disease (GERD), a risk factor for Barrett’s esophagus (BE), is a major concern in patients undergoing Sleeve gastrectomy (SG). In this meta-analysis, we assess the incidence of and analyze predictive factors for post-SG BE.
Methods: A literature search was conducted through April 2024 for studies reporting on incidence of BE, erosive esophagitis (EE) and hiatal hernia (HH) post-SG. Primary outcomes were post-SG pooled rates of de novo BE, EE, GERD symptoms, proton pump inhibitor (PPI) use and HH. Meta-regression analysis was performed to assess if patient and post-SG factors influenced the rates of post-SG BE.
Results: 19 studies with 2046 patients (79% females) were included in the final analysis. The mean age and mean follow-up ranged from 34.8-51 and 2-11.4 years (87.5-1491.7 person years), respectively. Overall, 240 patients were lost to follow up, and 1806 patients were included for post-SG analysis.
The pooled rate (PR) of de novo BE was 5.6% (95% CI 3.5-8.8) from 19 studies. In 3 studies with ≥ 10 years follow up, the PR of de novo BE was 11.6% (95% CI 5.9-21.5; I272).
The PR of GER/GERD symptoms pre- and post-SG was 14.6% (95% CI 10.6-19.9; I287) and 48% (95% CI 39.1-57; I291), respectively. There was a statistically significant increase in the risk of GER/GERD symptoms post-SG, Risk Ratio (RR) 3.32 (95% CI 2.35 - 4.67; I2 78); p< 0.001.
The PR of pre- and post-SG EE was 7.7% (95% CI 4.7-12.5; I282) and 33.4% (95% CI 26.6-40.9; I289). There was a statistically significant increase in the risk of EE post-SG, RR 3.37 (95% CI 2.49-4.58; I248); p< 0.001.
The PR of pre- and post-SG HH was 14.8% (95% CI 9.9-21.4; I279) and 32.1% (95% CI 21-45.6; I293). There was a statistically significant increase in the risk of HH post-SG, RR 2.09 (95% CI 1.5-2.9; I2 55); p< 0.001.
The PR of pre- and post-SG PPI use was 13.5% (95% CI 8.9-20; I275) and 54.6% (95% CI 46.2-62.7; I287). There was a statistically significant increase in PPI use post-SG, RR 3.65 (95% CI 2.25-5.93; I2 80); p< 0.001.
Based on meta-regression analysis, there was no influence of age, gender, pre- and post-operative BMI, post-procedure HH and EE on PR of post-SG BE. Post-SG GER/GERD had a negative correlation, indicating that incidence of post-SG BE was lower among patients with higher reported GER/GERD.
Discussion: Our analysis shows that SG results in a significantly increased risk of de novo BE and higher rates of EE, PPI use and HH. Hence, clinicians should routinely screen patients with SG for BE.
Disclosures:
Saurabh Chandan indicated no relevant financial relationships.
Shahab Khan indicated no relevant financial relationships.
Smit Deliwala indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Daryl Ramai indicated no relevant financial relationships.
Syed Saghir indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Lena Kassab indicated no relevant financial relationships.
Antonio Facciorusso indicated no relevant financial relationships.
Kalyana Nandipati indicated no relevant financial relationships.
Dennis Yang: 3D-Matrix – Consultant. Boston Scientific – Consultant. Fujifilm – Consultant. Medtronic – Consultant. Microtech – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Saurabh Chandan, MD1, Shahab Khan, MBBS2, Smit Deliwala, MD3, Dushyant S. Dahiya, MD4, Babu Mohan, MD5, Daryl Ramai, MD6, Syed Saghir, MD1, Banreet Dhindsa, MD7, Lena Kassab, MD8, Antonio Facciorusso, MD, PhD9, Kalyana Nandipati, MD10, Dennis Yang, MD11, Douglas Adler, MD12. P2216 - Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
