Monday Poster Session
Category: Esophagus
P2249 - Esophageal Obstruction Secondary to Gastric Intussusception of Hiatal Hernia: A Cathartic Reduction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Matt R. Pelton, MD
Rutgers Robert Wood Johnson University Hospital
New Brunswick, NJ
Presenting Author(s)
Award: Presidential Poster Award
Matt R. Pelton, MD1, Samuel Y. Jo, MD2, Anish V. Patel, MD2
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: In emergency department patients, epigastric pain is a common presenting symptom associated with a broad differential of etiologies. Here we report a case of gastro-gastric intussusception secondary to a hiatal hernia presenting with epigastric pain.
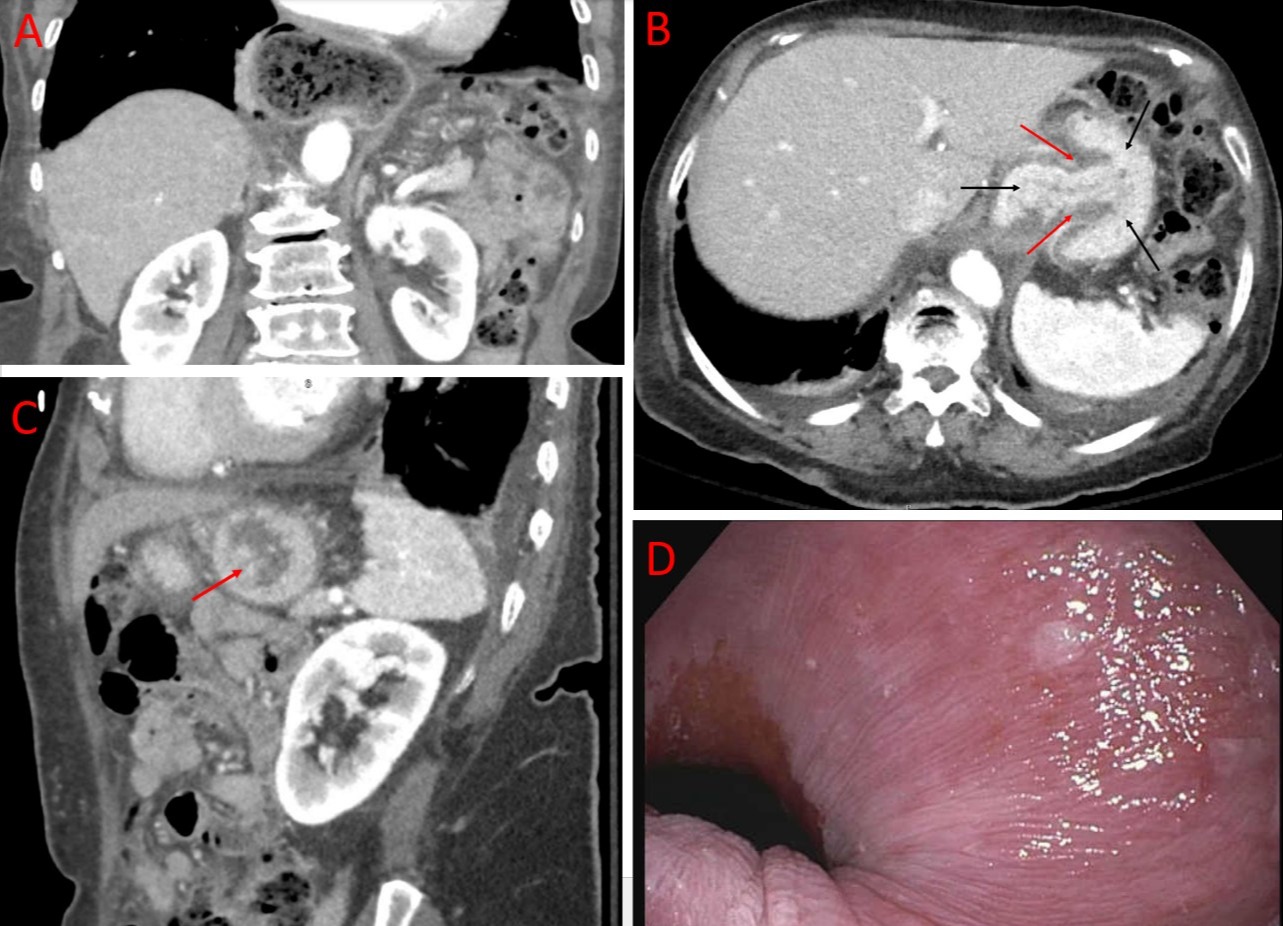
Case Description/Methods: An 86-year-old female with a history of gastroesophageal reflux disease and a small hiatal hernia presented with acute worsening of chronic epigastric pain. Vitals and labs on admission were within normal limits, excepting a leukocytosis and left shift. CT of her abdomen and pelvis demonstrated a dilated moderate-sized hiatal hernia containing debris (Figure 1A) with focal narrowing of the gastric lumen through the hiatus surrounded by gastric wall thickening (Figure 1B) and a positive ‘donut sign’ (Figure 1C) consistent with gastro-gastric intussusception. An urgent upper endoscopy was performed where food residue obstructing the distal esophagus and the hiatal hernia sac was able to be traversed accompanied by a tactile pop. The trapped food and debris were successfully cleared by irrigation, and the underlying hiatal hernia was reduced in size, measuring 2 cm with residual traction marks around the reduced gastric mucosa (Figure 1D). No mass or mucosal ischemia was noted. The patient’s symptoms resolved and a follow-up esophagogram showed a residual small hiatal hernia.
Discussion: Gastro-gastric intussusception is a rare presentation typically associated with a pathologic lead point such as a tumor, polyp, fundoplication, hiatal hernia, or gastroesophageal varices. Early diagnosis with imaging, and subsequent urgent intervention is essential. First-line treatment is endoscopic evaluation and reduction of the hernia to preserve the local blood supply and prevent ulceration or perforation. If an endoscopic evaluation is insufficient to reduce gastro-gastric intussusception, minimally invasive or invasive surgery may be necessary to salvage gastric blood supply. Once the intussusception has resolved, patients should have the pathologic lead point resected or repaired due to high rates of recurrent symptoms without correction. Depending on the location and nature of the lead point, gastro-jejunal anastomosis, subtotal gastrectomy, or hernia repair may be considered appropriate. The case presented here was arranged to have outpatient high-resolution manometry completed to plan for surgical hernia repair.
Disclosures:
Matt R. Pelton, MD1, Samuel Y. Jo, MD2, Anish V. Patel, MD2. P2249 - Esophageal Obstruction Secondary to Gastric Intussusception of Hiatal Hernia: A Cathartic Reduction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Matt R. Pelton, MD1, Samuel Y. Jo, MD2, Anish V. Patel, MD2
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: In emergency department patients, epigastric pain is a common presenting symptom associated with a broad differential of etiologies. Here we report a case of gastro-gastric intussusception secondary to a hiatal hernia presenting with epigastric pain.
Case Description/Methods: An 86-year-old female with a history of gastroesophageal reflux disease and a small hiatal hernia presented with acute worsening of chronic epigastric pain. Vitals and labs on admission were within normal limits, excepting a leukocytosis and left shift. CT of her abdomen and pelvis demonstrated a dilated moderate-sized hiatal hernia containing debris (Figure 1A) with focal narrowing of the gastric lumen through the hiatus surrounded by gastric wall thickening (Figure 1B) and a positive ‘donut sign’ (Figure 1C) consistent with gastro-gastric intussusception. An urgent upper endoscopy was performed where food residue obstructing the distal esophagus and the hiatal hernia sac was able to be traversed accompanied by a tactile pop. The trapped food and debris were successfully cleared by irrigation, and the underlying hiatal hernia was reduced in size, measuring 2 cm with residual traction marks around the reduced gastric mucosa (Figure 1D). No mass or mucosal ischemia was noted. The patient’s symptoms resolved and a follow-up esophagogram showed a residual small hiatal hernia.
Discussion: Gastro-gastric intussusception is a rare presentation typically associated with a pathologic lead point such as a tumor, polyp, fundoplication, hiatal hernia, or gastroesophageal varices. Early diagnosis with imaging, and subsequent urgent intervention is essential. First-line treatment is endoscopic evaluation and reduction of the hernia to preserve the local blood supply and prevent ulceration or perforation. If an endoscopic evaluation is insufficient to reduce gastro-gastric intussusception, minimally invasive or invasive surgery may be necessary to salvage gastric blood supply. Once the intussusception has resolved, patients should have the pathologic lead point resected or repaired due to high rates of recurrent symptoms without correction. Depending on the location and nature of the lead point, gastro-jejunal anastomosis, subtotal gastrectomy, or hernia repair may be considered appropriate. The case presented here was arranged to have outpatient high-resolution manometry completed to plan for surgical hernia repair.
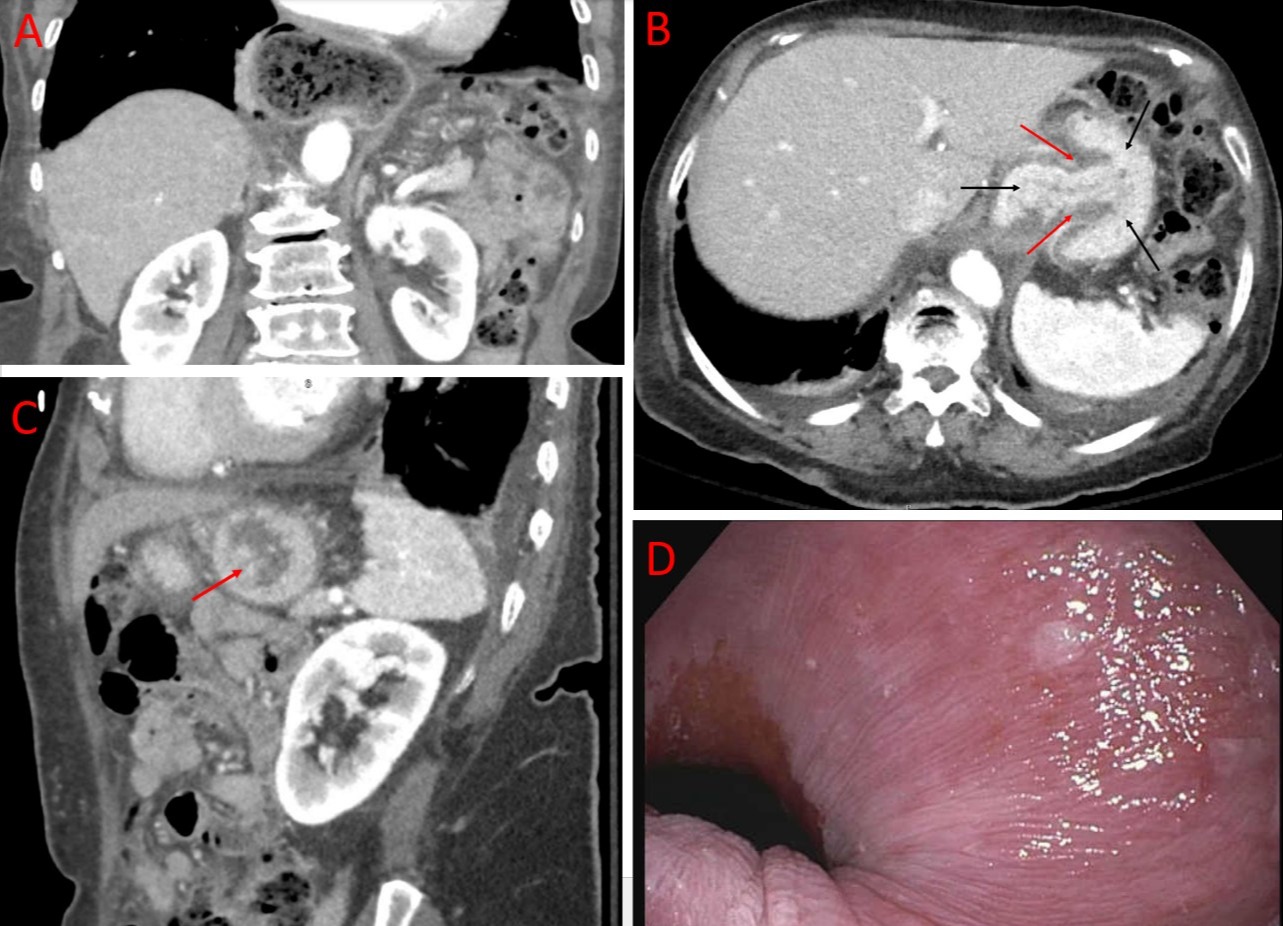
Figure: CT scan with different views demonstrating A) dilated moderate-sized hiatal hernia containing debris, B) focal narrowing of the gastric lumen through the hiatus around the area of gastric wall thickening and intussusception, C) classic doughnut sign of gastro-gastric intussusception and D) endoscopic view after decompression of remaining hiatal hernia after reduction.
Disclosures:
Matt Pelton indicated no relevant financial relationships.
Samuel Jo indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Matt R. Pelton, MD1, Samuel Y. Jo, MD2, Anish V. Patel, MD2. P2249 - Esophageal Obstruction Secondary to Gastric Intussusception of Hiatal Hernia: A Cathartic Reduction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

