Monday Poster Session
Category: Esophagus
P2254 - Giant Mediastinal Hemangioma with Esophageal Involvement Causing Food Impaction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lawrence Zhou, MD
The University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Lawrence Zhou, MD1, John Thesing, DO2, Aastha V. Bharwad, MD2, Maurice Kliewer, MD3, Kyle Rowe, MD4
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Robert J. Dole Veterans Affairs Medical Center, Wichita, KS; 4University of Kansas Medical Center, Wichita, KS
Introduction: Mediastinal hemangiomas are very rare benign tumors, making up 0.5% of mediastinal tumors and are more common before 35 years of age. They occur more frequently in the anterior, followed by the posterior compartment, and are histologically classified into cavernous, capillary, and venous types. They are usually well-circumscribed, but can also infiltrate into surrounding structures, necessitating surgical excision. They may present in a variety of ways, such as a cough, mild dyspnea, respiratory distress, or chest pain.
Case Description/Methods: A 61-year-old male with reported history of large mediastinal hemangioma incidentally discovered 25 years prior on routine imaging presented to the ED for overnight abdominal pressure, dysphagia, and globus sensation. The patient had previously opted against surgical excision and noted worsening dysphagia over the past year.
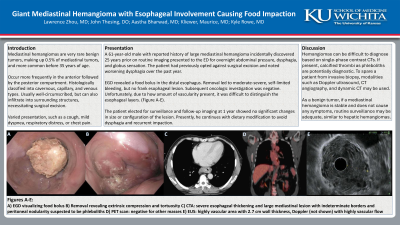
He underwent esophagogastroduodenoscopy, which revealed a food bolus in the distal esophagus. Removal led to moderate-severe, self-limited bleeding and revealed extrinsic compression and tortuosity of the distal esophagus, suspected to be due to the known mediastinal lesion (Figure A-B). There was no frank esophageal erosion. Torso computed tomography (CT) angiography showed severe esophageal thickening and large mediastinal lesion with indeterminate borders and peritoneal nodularity, concerning for malignancy (Figure C). Fortunately, positron emission tomography did not find other masses (Figure D). The peritoneal nodularity was suspected to be phleboliths. Endoscopic ultrasound showed wall thickness of 2.7 cm and highly vascular area on Doppler flow, making the esophageal layers difficult to determine (Figure E). The stomach had diffuse, moderate inflammation with numerous telangiectasis.
The patient elected for surveillance. Follow-up imaging at 1 year showed no significant changes in size or configuration of the lesion. He continues with dietary modification to avoid dysphagia and recurrent impaction.
Discussion: Hemangiomas must be included in the differential diagnosis of hypervascular masses, but can be difficult to diagnose based on single-phase contrast CTs. If present, calcified thrombi as phleboliths are potentially diagnostic. To spare a patient from invasive biopsy, modalities such as Doppler ultrasound, CT angiography, and dynamic CT may be used. As a benign tumor, if a mediastinal hemangioma is stable and does not cause any symptoms, routine surveillance may be adequate, similar to guidance for hepatic hemangiomas.
Disclosures:
Lawrence Zhou, MD1, John Thesing, DO2, Aastha V. Bharwad, MD2, Maurice Kliewer, MD3, Kyle Rowe, MD4. P2254 - Giant Mediastinal Hemangioma with Esophageal Involvement Causing Food Impaction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Robert J. Dole Veterans Affairs Medical Center, Wichita, KS; 4University of Kansas Medical Center, Wichita, KS
Introduction: Mediastinal hemangiomas are very rare benign tumors, making up 0.5% of mediastinal tumors and are more common before 35 years of age. They occur more frequently in the anterior, followed by the posterior compartment, and are histologically classified into cavernous, capillary, and venous types. They are usually well-circumscribed, but can also infiltrate into surrounding structures, necessitating surgical excision. They may present in a variety of ways, such as a cough, mild dyspnea, respiratory distress, or chest pain.
Case Description/Methods: A 61-year-old male with reported history of large mediastinal hemangioma incidentally discovered 25 years prior on routine imaging presented to the ED for overnight abdominal pressure, dysphagia, and globus sensation. The patient had previously opted against surgical excision and noted worsening dysphagia over the past year.
He underwent esophagogastroduodenoscopy, which revealed a food bolus in the distal esophagus. Removal led to moderate-severe, self-limited bleeding and revealed extrinsic compression and tortuosity of the distal esophagus, suspected to be due to the known mediastinal lesion (Figure A-B). There was no frank esophageal erosion. Torso computed tomography (CT) angiography showed severe esophageal thickening and large mediastinal lesion with indeterminate borders and peritoneal nodularity, concerning for malignancy (Figure C). Fortunately, positron emission tomography did not find other masses (Figure D). The peritoneal nodularity was suspected to be phleboliths. Endoscopic ultrasound showed wall thickness of 2.7 cm and highly vascular area on Doppler flow, making the esophageal layers difficult to determine (Figure E). The stomach had diffuse, moderate inflammation with numerous telangiectasis.
The patient elected for surveillance. Follow-up imaging at 1 year showed no significant changes in size or configuration of the lesion. He continues with dietary modification to avoid dysphagia and recurrent impaction.
Discussion: Hemangiomas must be included in the differential diagnosis of hypervascular masses, but can be difficult to diagnose based on single-phase contrast CTs. If present, calcified thrombi as phleboliths are potentially diagnostic. To spare a patient from invasive biopsy, modalities such as Doppler ultrasound, CT angiography, and dynamic CT may be used. As a benign tumor, if a mediastinal hemangioma is stable and does not cause any symptoms, routine surveillance may be adequate, similar to guidance for hepatic hemangiomas.
Figure: Figure A - Food bolus in distal esophagus. Figure B - Distal esophagus after removal of food bolus. Figure C - Computed tomography, level of distal esophagus. Figure D - Positron emission tomography. Figure E - Endoscopic ultrasound of distal esophagus.
Disclosures:
Lawrence Zhou indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Maurice Kliewer indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
Lawrence Zhou, MD1, John Thesing, DO2, Aastha V. Bharwad, MD2, Maurice Kliewer, MD3, Kyle Rowe, MD4. P2254 - Giant Mediastinal Hemangioma with Esophageal Involvement Causing Food Impaction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
