Monday Poster Session
Category: Esophagus
P2263 - A Case of Opioid-Induced Esophageal Dysmotility (OIED) in the Setting of Hypermobile Ehlers-Danlos Syndrome (hEDS)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Theja Channapragada, DO, MBA, MS
Penn State Health Milton S. Hershey Medical Center
Springfield, NJ
Presenting Author(s)
Theja Channapragada, DO, MBA, MS1, Zubair Malik, MD2, Abirami Rajendiran, MD3, Srinivas Channapragada, MD4
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Virtua Health System, Voorhees, NJ; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Springfield, NJ
Introduction: OIED is defined by esophageal symptoms and specific manometric abnormalities associated with chronic opioid use. Hypermobile Ehlers-Danlos syndrome (hEDS) is a heritable connective tissue disorder with a high symptom burden, including gastrointestinal symptoms, such as dysphagia. Patients may undergo innumerable diagnostic tests and may require opioids for pain management. The presentation of OIED in the setting of hEDS warrants further review.
Case Description/Methods: A 51-year-old Caucasian female with hEDS presented with a chronic history of nausea, vomiting, bloating, early satiety, and abdominal pain. She recently experienced dysphagia primarily for solid foods, with no weight loss. She was on opioid therapy for her musculoskeletal symptoms. She was on oxycodone for over ten years and transitioned to buprenorphine more recently. The diagnosis of hEDS was confirmed with Beighton Score.
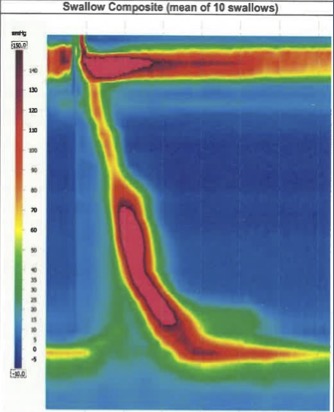
Upper Endoscopy and endoscopic ultrasound revealed narrowing of the distal esophagus, with no inflammation. High-resolution esophageal manometry (HRM) identified an esophagogastric junction outflow obstruction (EGJOO)(See Figure). A subsequent study using functional lumen imaging probe (FLIP) revealed repetitive anterograde contractions (RACs) and contractile activity with spastic and/or reactive features. Reduced esophagogastric junction opening and abnormal contractility of the esophagus were noted, which confirmed the HRM findings. Botulinum toxin was administered which significantly improved her dysphagia.
Discussion: This case highlights a possible association between hEDS and OIED. Upper GI symptoms, including dysphagia, are frequently seen in hEDS patients, even in those who are not on opioids. In hEDS, changes in neuronal function and modification of gastrointestinal wall compliance may contribute to esophageal dysmotility. Chronic opioid use possibly increases excitatory signals in the esophagus causing abnormal esophageal body movement and impaired relaxation of the lower esophageal sphincter (LES), contributing to OIED. HRM diagnoses spastic and obstructive abnormalities in OIED such as EGJOO. Furthermore, FLIP may be more tolerated by patients than HRM and may reveal an increase in repetitive retrograde contractions or abnormal distensibility of the LES in chronic opioid users. Oxycodone and hydrocodone have a higher prevalence of inducing OIED compared to weaker opioids such as tramadol. Botulinum toxin injection is a treatment option, particularly for patients who cannot discontinue opioids.
Disclosures:
Theja Channapragada, DO, MBA, MS1, Zubair Malik, MD2, Abirami Rajendiran, MD3, Srinivas Channapragada, MD4. P2263 - A Case of Opioid-Induced Esophageal Dysmotility (OIED) in the Setting of Hypermobile Ehlers-Danlos Syndrome (hEDS), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Virtua Health System, Voorhees, NJ; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Springfield, NJ
Introduction: OIED is defined by esophageal symptoms and specific manometric abnormalities associated with chronic opioid use. Hypermobile Ehlers-Danlos syndrome (hEDS) is a heritable connective tissue disorder with a high symptom burden, including gastrointestinal symptoms, such as dysphagia. Patients may undergo innumerable diagnostic tests and may require opioids for pain management. The presentation of OIED in the setting of hEDS warrants further review.
Case Description/Methods: A 51-year-old Caucasian female with hEDS presented with a chronic history of nausea, vomiting, bloating, early satiety, and abdominal pain. She recently experienced dysphagia primarily for solid foods, with no weight loss. She was on opioid therapy for her musculoskeletal symptoms. She was on oxycodone for over ten years and transitioned to buprenorphine more recently. The diagnosis of hEDS was confirmed with Beighton Score.
Upper Endoscopy and endoscopic ultrasound revealed narrowing of the distal esophagus, with no inflammation. High-resolution esophageal manometry (HRM) identified an esophagogastric junction outflow obstruction (EGJOO)(See Figure). A subsequent study using functional lumen imaging probe (FLIP) revealed repetitive anterograde contractions (RACs) and contractile activity with spastic and/or reactive features. Reduced esophagogastric junction opening and abnormal contractility of the esophagus were noted, which confirmed the HRM findings. Botulinum toxin was administered which significantly improved her dysphagia.
Discussion: This case highlights a possible association between hEDS and OIED. Upper GI symptoms, including dysphagia, are frequently seen in hEDS patients, even in those who are not on opioids. In hEDS, changes in neuronal function and modification of gastrointestinal wall compliance may contribute to esophageal dysmotility. Chronic opioid use possibly increases excitatory signals in the esophagus causing abnormal esophageal body movement and impaired relaxation of the lower esophageal sphincter (LES), contributing to OIED. HRM diagnoses spastic and obstructive abnormalities in OIED such as EGJOO. Furthermore, FLIP may be more tolerated by patients than HRM and may reveal an increase in repetitive retrograde contractions or abnormal distensibility of the LES in chronic opioid users. Oxycodone and hydrocodone have a higher prevalence of inducing OIED compared to weaker opioids such as tramadol. Botulinum toxin injection is a treatment option, particularly for patients who cannot discontinue opioids.
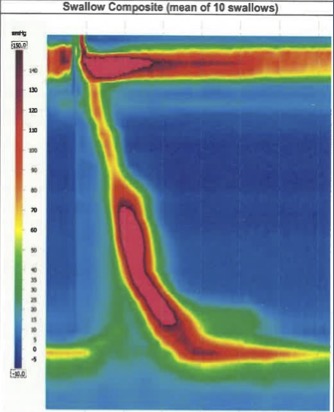
Figure: High-resolution esophageal manometry (HRM) identifying esophagogastric junction outflow obstruction (EGJOO).
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Zubair Malik indicated no relevant financial relationships.
Abirami Rajendiran indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
Theja Channapragada, DO, MBA, MS1, Zubair Malik, MD2, Abirami Rajendiran, MD3, Srinivas Channapragada, MD4. P2263 - A Case of Opioid-Induced Esophageal Dysmotility (OIED) in the Setting of Hypermobile Ehlers-Danlos Syndrome (hEDS), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
