Monday Poster Session
Category: Esophagus
P2264 - An Unusual Cause of Food Impaction: Neuroendocrine Tumor
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Christine Son, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Christine Son, MD1, Daniel Havlichek, MD1, Jeff Leya, MD2, Josh Kalapala, BSc3, Promila Banerjee, MD, FACG3
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL; 3Edwards Hines Jr. VA Hospital, Maywood, IL
Introduction: Esophageal neuroendocrine carcinomas (ENECs) can arise in any body organ but only 1.6% are found in the esophagus (1). Given the rarity, disease characteristics and standard treatment are not well defined. We present a case of large obstructive ENEC with excellent treatment response.
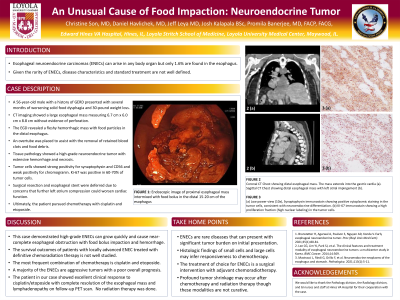
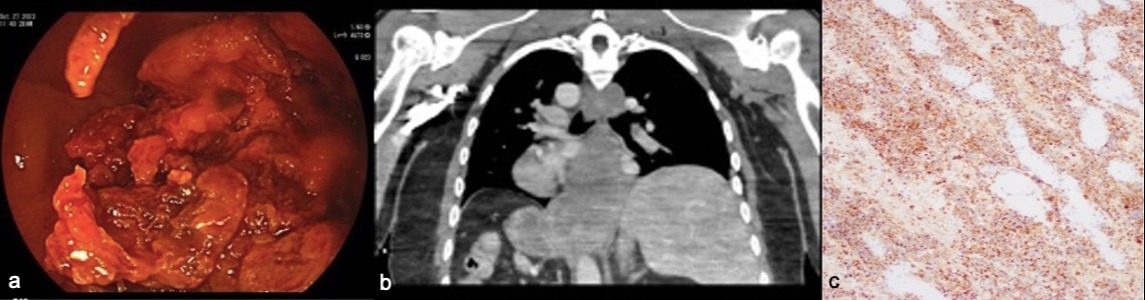
Case Description/Methods: A 56-year-old male with a history of GERD presented with worsening solid food dysphagia and 30-pound weight loss. CT imaging showed a large esophageal mass measuring 6.7 cm x 6.0 cm x 8.8 cm without evidence of perforation. The EGD revealed a fleshy hemorrhagic mass with food particles in the distal esophagus. An overtube was placed to assist with the removal of retained blood clots and food debris. Pathology showed a high-grade neuroendocrine tumor with extensive hemorrhage and necrosis. The surgery and esophageal stent were deferred due to concerns that further left atrium compression could worsen cardiac function. Ultimately, the patient pursued radiation and chemotherapy with cisplatin and etoposide.
Discussion: Given the rarity of ENECs, the survival outcome of patients with locally advanced disease treated with definitive chemoradiation therapy is not well studied. The most frequent combination of chemotherapy used was cisplatin and etoposide (2). A majority of the ENECs show aggressive behavior with poor overall prognosis (3).
This case is unique because of the rarity of ENEC, the significant tumor burden on presentation, and the mass effect on the heart causing complications of cardiac arrhythmias that precluded esophageal stent placement. The case also required multiple endoscopies including an overtube use to clear the esophagus of food and clot, and to diagnose the underlying malignancy. This case raises awareness that not all obstructive esophageal tumors need stents. The patient completed 4 cycles of cisplatin/etoposide with PET scan showing complete resolution of the esophageal mass and lymphadenopathy. The patient will continue surveillance PET scan with EGD with plans to proceed with salvage esophagectomy if the disease recurs.
References
1. Branstetter H, Agarwal A, Paulson S, Nguyen AD, Konda V. Early esophageal neuroendocrine tumor. Proc (Bayl Univ Med Cent). 2021;35(1):80-81.
2. Lee CG, Lim YJ, Park SJ, et al. The clinical features and treatment modality of esophageal neuroendocrine tumors: a multicenter study in Korea. BMC Cancer. 2014;14:569.
3. Mastracci L, Rindi G, Grillo F, et al. Neuroendocrine neoplasms of the esophagus and stomach. Pathologica. 2021;113(1):5-11.
Disclosures:
Christine Son, MD1, Daniel Havlichek, MD1, Jeff Leya, MD2, Josh Kalapala, BSc3, Promila Banerjee, MD, FACG3. P2264 - An Unusual Cause of Food Impaction: Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL; 3Edwards Hines Jr. VA Hospital, Maywood, IL
Introduction: Esophageal neuroendocrine carcinomas (ENECs) can arise in any body organ but only 1.6% are found in the esophagus (1). Given the rarity, disease characteristics and standard treatment are not well defined. We present a case of large obstructive ENEC with excellent treatment response.
Case Description/Methods: A 56-year-old male with a history of GERD presented with worsening solid food dysphagia and 30-pound weight loss. CT imaging showed a large esophageal mass measuring 6.7 cm x 6.0 cm x 8.8 cm without evidence of perforation. The EGD revealed a fleshy hemorrhagic mass with food particles in the distal esophagus. An overtube was placed to assist with the removal of retained blood clots and food debris. Pathology showed a high-grade neuroendocrine tumor with extensive hemorrhage and necrosis. The surgery and esophageal stent were deferred due to concerns that further left atrium compression could worsen cardiac function. Ultimately, the patient pursued radiation and chemotherapy with cisplatin and etoposide.
Discussion: Given the rarity of ENECs, the survival outcome of patients with locally advanced disease treated with definitive chemoradiation therapy is not well studied. The most frequent combination of chemotherapy used was cisplatin and etoposide (2). A majority of the ENECs show aggressive behavior with poor overall prognosis (3).
This case is unique because of the rarity of ENEC, the significant tumor burden on presentation, and the mass effect on the heart causing complications of cardiac arrhythmias that precluded esophageal stent placement. The case also required multiple endoscopies including an overtube use to clear the esophagus of food and clot, and to diagnose the underlying malignancy. This case raises awareness that not all obstructive esophageal tumors need stents. The patient completed 4 cycles of cisplatin/etoposide with PET scan showing complete resolution of the esophageal mass and lymphadenopathy. The patient will continue surveillance PET scan with EGD with plans to proceed with salvage esophagectomy if the disease recurs.
References
1. Branstetter H, Agarwal A, Paulson S, Nguyen AD, Konda V. Early esophageal neuroendocrine tumor. Proc (Bayl Univ Med Cent). 2021;35(1):80-81.
2. Lee CG, Lim YJ, Park SJ, et al. The clinical features and treatment modality of esophageal neuroendocrine tumors: a multicenter study in Korea. BMC Cancer. 2014;14:569.
3. Mastracci L, Rindi G, Grillo F, et al. Neuroendocrine neoplasms of the esophagus and stomach. Pathologica. 2021;113(1):5-11.
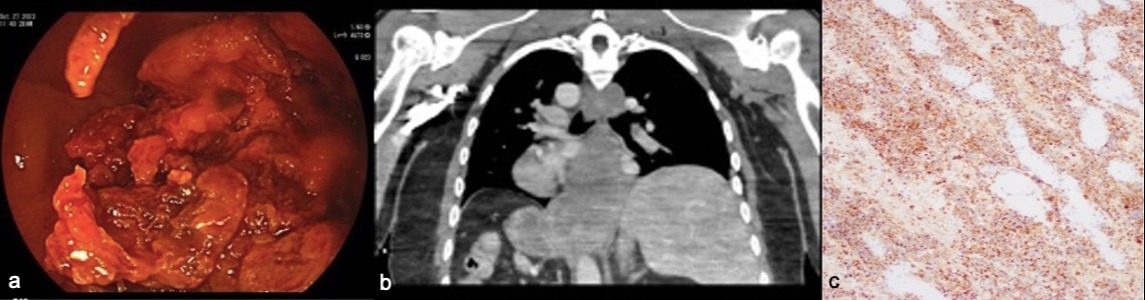
Figure: The initial endoscopic image of proximal esophageal mass intermixed with food bolus in the distal 15-20 cm of the esophagus (a).
Coronal CT Chest showing distal esophageal mass. The mass is extending into the gastric cardia measuring 6.7 cm x 6.0 cm x 8.8 cm without evidence of perforation (b).
Low power view (10x), Synaptophysin immunostained slide showing positive cytoplasmic staining in the tumor cells, consistent with neuroendocrine differentiation (c).
Coronal CT Chest showing distal esophageal mass. The mass is extending into the gastric cardia measuring 6.7 cm x 6.0 cm x 8.8 cm without evidence of perforation (b).
Low power view (10x), Synaptophysin immunostained slide showing positive cytoplasmic staining in the tumor cells, consistent with neuroendocrine differentiation (c).
Disclosures:
Christine Son indicated no relevant financial relationships.
Daniel Havlichek indicated no relevant financial relationships.
Jeff Leya indicated no relevant financial relationships.
Josh Kalapala indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Christine Son, MD1, Daniel Havlichek, MD1, Jeff Leya, MD2, Josh Kalapala, BSc3, Promila Banerjee, MD, FACG3. P2264 - An Unusual Cause of Food Impaction: Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
