Monday Poster Session
Category: Esophagus
P2266 - Interplay of Hypereosinophilic Syndrome (HES) With Serosal Eosinophilic Gastroenteritis (EGE)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aadhithyaraman Santharaman, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Award: Presidential Poster Award
Aadhithyaraman Santharaman, MD1, Archit Garg, MD2, Sahil Raval, MD1, Vishali Moond, MD1, Mohamed Riaz, MBBS3, Sugirdhana Velpari, MD1, Arkady Broder, MD2, Debra Goldstein, MD1
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Kuwait Ministry of Health, Adan Hospital, Manipal, Al Ahmadi, Kuwait
Introduction: Eosinophilic gastroenteritis (EGE) is a rare inflammatory disorder with eosinophilic infiltration of the gastrointestinal tract. According to the Klein classification, EGE is sub-divided into mucosal, muscular, and serosal subtype. The latter is characterized by significant peripheral eosinophilia and eosinophilic ascites. We present a unique case of serosal EGE with exceptionally high peripheral eosinophilia, diagnosed as hypereosinophilic syndrome (HES).
Case Description/Methods: A 68-year-old woman presented with two weeks of abdominal distension, bloating, nausea, reflux, and frequent small-volume diarrhea (10-15 times daily). She had also had a loss of appetite and unintentional weight loss of 10-15 lbs during this period. One month ago, she visited Hawaii for a week. Her WBC count upon presentation was 47,500 cells/mm3 with 74% eosinophils (eos). Imaging showed diffuse wall thickening of esophagus and multiple small bowel loops, moderate ascites and a small right pleural effusion.
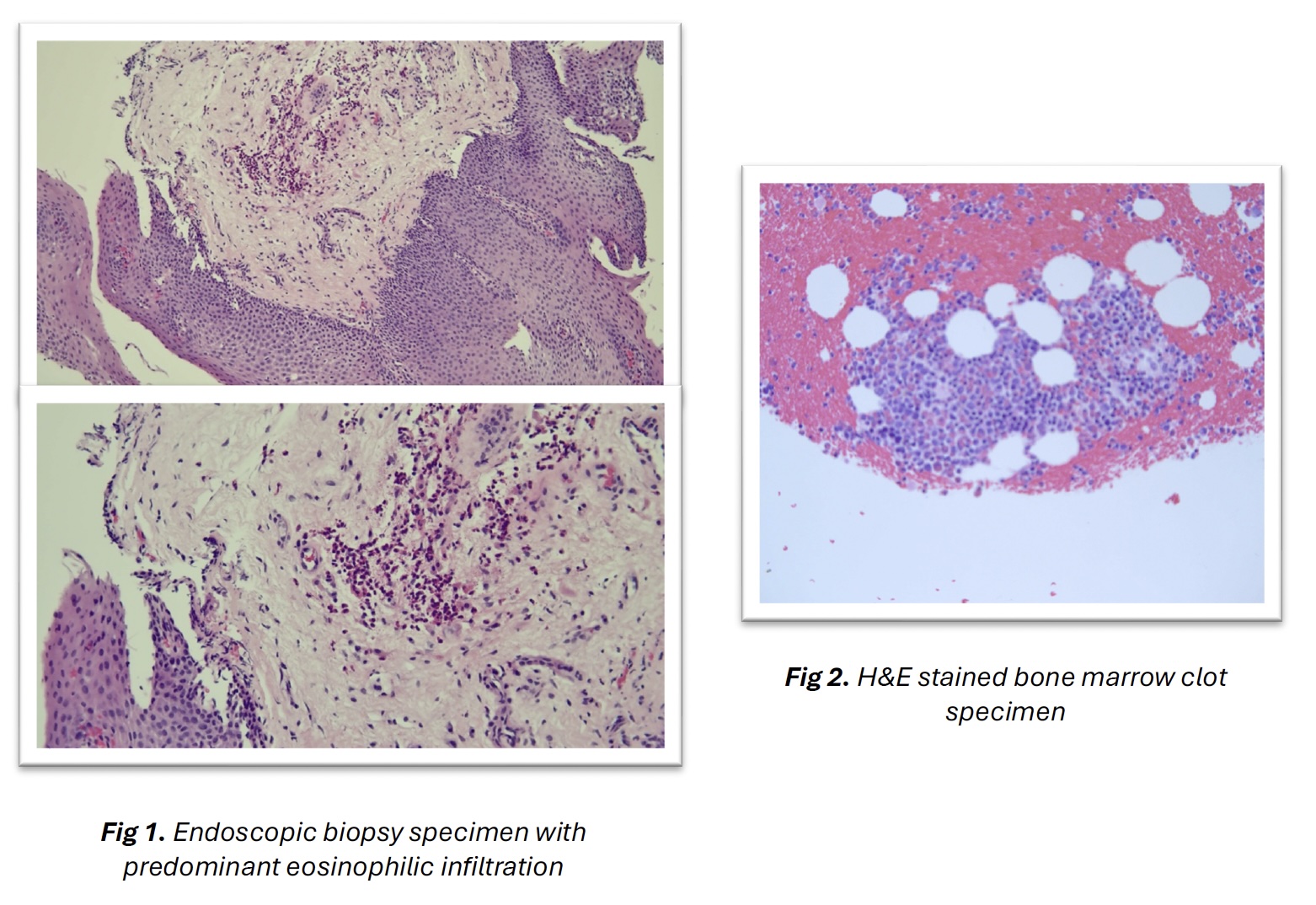
Upper endoscopy and flexible sigmoidoscopy revealed an eosinophilic infiltration in the esophagus (7 eos/hpf), descending colon, sigmoid colon, and most notably in the rectum. Infectious work-up of the bowel was negative, including ova and parasites. Serology was negative for Strongyloides and Trichinella. Serum IgE was elevated at 1161 kU/L, serum tryptase was normal, ANCA was negative. Paracentesis was eosinophil-predominant (8517 cells/mm3), culture and adenosine deaminase were negative.
Except for the initial IV antibiotics, the patient was managed supportively with PPI 40 mg daily. She was discharged after a bone marrow biopsy, which revealed HES without mastocytosis or neoplasm. FISH testing was negative for the FIP1L1::PDGFRA fusion mutation. One week later, she was started on oral prednisone 50 mg daily. Her symptoms improved markedly within 5 days.
Discussion: Distinguishing between HES and EGE can be challenging. This is especially true in early stages, if HES is confined to a single organ, the gastrointestinal tract as in this case. Corticosteroids are the primary initial treatment for both FIP1L1::PDGFRA-negative HES and EGE. Our patient has predictors for chronic disease requiring ongoing medication: weight loss, hypoalbuminemia, serosal involvement, and anemia at diagnosis. Gastroenterologists must be vigilant in identifying HES in EGE cases with marked peripheral eosinophilia, as HES can affect multiple organs. Early management is crucial, as a missed diagnosis can be fatal.
Disclosures:
Aadhithyaraman Santharaman, MD1, Archit Garg, MD2, Sahil Raval, MD1, Vishali Moond, MD1, Mohamed Riaz, MBBS3, Sugirdhana Velpari, MD1, Arkady Broder, MD2, Debra Goldstein, MD1. P2266 - Interplay of Hypereosinophilic Syndrome (HES) With Serosal Eosinophilic Gastroenteritis (EGE), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Aadhithyaraman Santharaman, MD1, Archit Garg, MD2, Sahil Raval, MD1, Vishali Moond, MD1, Mohamed Riaz, MBBS3, Sugirdhana Velpari, MD1, Arkady Broder, MD2, Debra Goldstein, MD1
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Kuwait Ministry of Health, Adan Hospital, Manipal, Al Ahmadi, Kuwait
Introduction: Eosinophilic gastroenteritis (EGE) is a rare inflammatory disorder with eosinophilic infiltration of the gastrointestinal tract. According to the Klein classification, EGE is sub-divided into mucosal, muscular, and serosal subtype. The latter is characterized by significant peripheral eosinophilia and eosinophilic ascites. We present a unique case of serosal EGE with exceptionally high peripheral eosinophilia, diagnosed as hypereosinophilic syndrome (HES).
Case Description/Methods: A 68-year-old woman presented with two weeks of abdominal distension, bloating, nausea, reflux, and frequent small-volume diarrhea (10-15 times daily). She had also had a loss of appetite and unintentional weight loss of 10-15 lbs during this period. One month ago, she visited Hawaii for a week. Her WBC count upon presentation was 47,500 cells/mm3 with 74% eosinophils (eos). Imaging showed diffuse wall thickening of esophagus and multiple small bowel loops, moderate ascites and a small right pleural effusion.
Upper endoscopy and flexible sigmoidoscopy revealed an eosinophilic infiltration in the esophagus (7 eos/hpf), descending colon, sigmoid colon, and most notably in the rectum. Infectious work-up of the bowel was negative, including ova and parasites. Serology was negative for Strongyloides and Trichinella. Serum IgE was elevated at 1161 kU/L, serum tryptase was normal, ANCA was negative. Paracentesis was eosinophil-predominant (8517 cells/mm3), culture and adenosine deaminase were negative.
Except for the initial IV antibiotics, the patient was managed supportively with PPI 40 mg daily. She was discharged after a bone marrow biopsy, which revealed HES without mastocytosis or neoplasm. FISH testing was negative for the FIP1L1::PDGFRA fusion mutation. One week later, she was started on oral prednisone 50 mg daily. Her symptoms improved markedly within 5 days.
Discussion: Distinguishing between HES and EGE can be challenging. This is especially true in early stages, if HES is confined to a single organ, the gastrointestinal tract as in this case. Corticosteroids are the primary initial treatment for both FIP1L1::PDGFRA-negative HES and EGE. Our patient has predictors for chronic disease requiring ongoing medication: weight loss, hypoalbuminemia, serosal involvement, and anemia at diagnosis. Gastroenterologists must be vigilant in identifying HES in EGE cases with marked peripheral eosinophilia, as HES can affect multiple organs. Early management is crucial, as a missed diagnosis can be fatal.
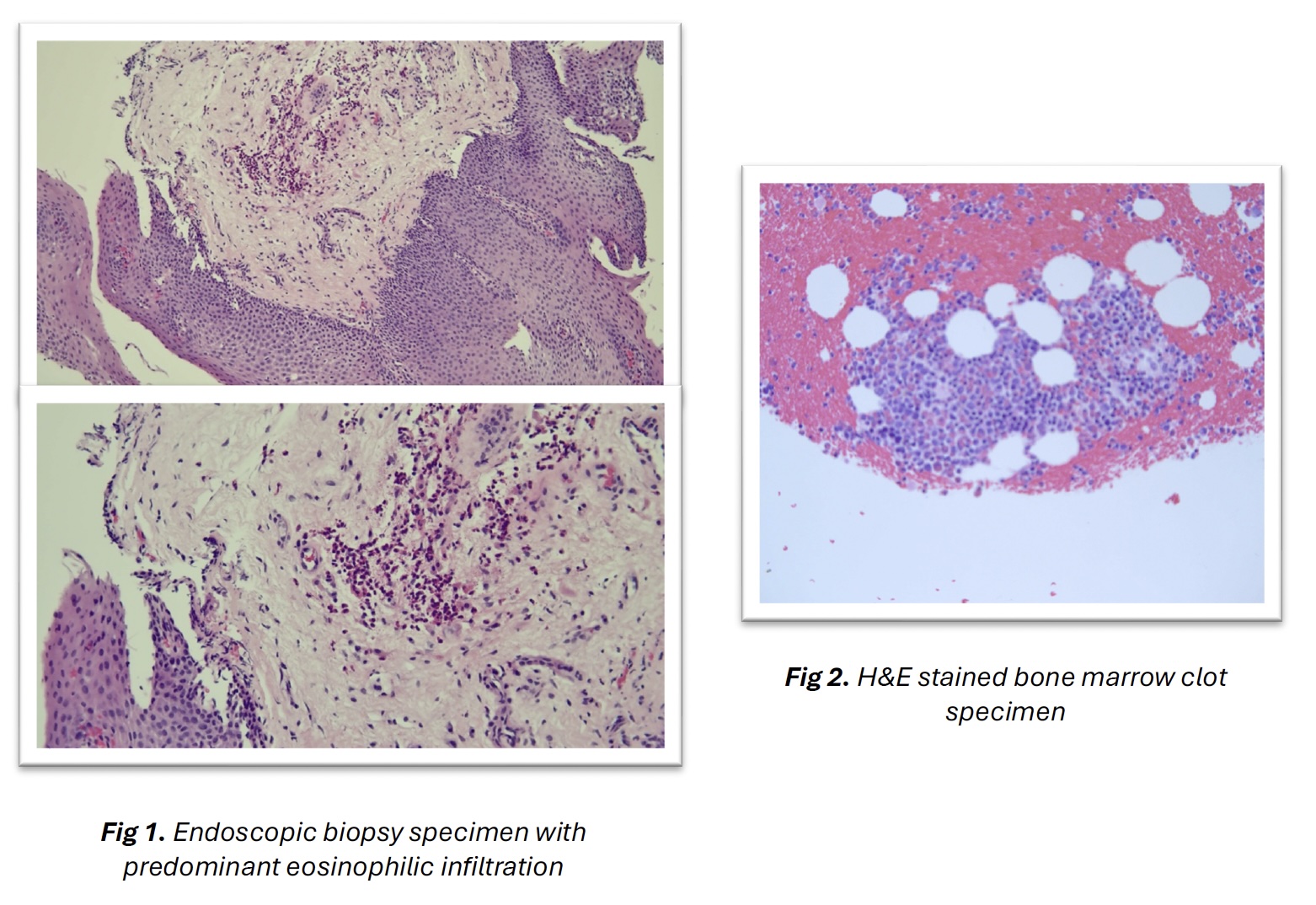
Figure: Fig 1. Endoscopic biopsy specimen with predominant eosinophilic infiltration, Fig 2. H&E stained bone marrow clot specimen
Disclosures:
Aadhithyaraman Santharaman indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Sahil Raval indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Mohamed Riaz indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Debra Goldstein indicated no relevant financial relationships.
Aadhithyaraman Santharaman, MD1, Archit Garg, MD2, Sahil Raval, MD1, Vishali Moond, MD1, Mohamed Riaz, MBBS3, Sugirdhana Velpari, MD1, Arkady Broder, MD2, Debra Goldstein, MD1. P2266 - Interplay of Hypereosinophilic Syndrome (HES) With Serosal Eosinophilic Gastroenteritis (EGE), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

