Monday Poster Session
Category: Esophagus
P2269 - From Dysphagia to Diagnosis: An Esophageal Enigma in a Post-Bacteremia Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Sayed T. Shah
University of Nicosia Medical School
Abbotsford, BC, Canada
Presenting Author(s)
Ahmad Sandouka, 1, Sayed T. Shah, 2, Mohammed W Khaled, MD3, Barakat Aburajab Altamimi, MD4
1University of Nicosia St. George's Medical School, Nicosia, Nicosia, Cyprus; 2University of Nicosia Medical School, Abbotsford, BC, Canada; 3King Hussein Medical Center, Amman, 'Amman, Jordan; 4Mercy Medical Center, Cedar Rapids, IA
Introduction: Esophageal abscess is a condition, when there is a buildup of pus within the esophagus. Severe chest discomfort, fever, and trouble swallowing are symptoms of esophageal abscesses. This can be caused by trauma, infections, or perforations. To avoid further complications like sepsis and mediastinitis, It can be diagnosed by imaging and treatment with antibiotics as well as drainage is critical.
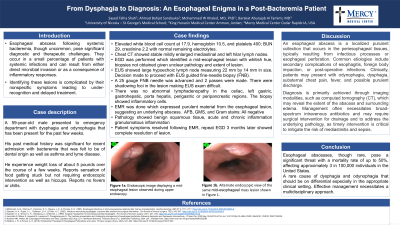
Case Description/Methods: A 59-year-old male, who had Lyme disease and asthma visited the ER with painful dysphagia. A month prior, he had received treatment for bacteremia, likely related to dental issues. Antibiotics initially helped to improve his condition, but a few days prior to his latest ER visit, he experienced a recurrence of his symptoms, which included significant chest pressure and recurrent hiccups. Mildly enlarged mediastinal and left hilar lymph nodes were discovered on a prior CT scan of the chest. The patient went back to the ER and complained of losing five pounds since his last hospital admission, difficulty swallowing, and the feeling that food was lodged in his esophagus. Abdominal pain, chills, nausea, vomiting, diarrhea, fever, and night sweats were all denied by him. The over-the-counter antacids did not work. Through an esophagogastroduodenoscopy (EGD) a mid-esophageal lesion was discovered. An endoscopic ultrasonography (EUS) detected a sizable hypoechoic lymph node (22 mm by 14 mm) in station 4L. With shadowing foci, the esophageal lesion at 30 cm from the incisura seemed superficial to the muscularis propria. There was no abnormal lymphadenopathy in the areas. An abscess was discovered during an endoscopic mucosal resection (EMR), which revealed purulent material from the lesion. After his lesion was removed, later a biopsy of the base revealed no perforation. Pathology confirmed that the lymph node did not contain any cancer cells and that there was benign squamous mucosa with acute, chronic, and granulomatous inflammation. Following the EMR, the patient's symptoms were resolved. An EGD three months later revealed no residual lesion.
Discussion: In this case, the presence of purulent material depicted an infectious or inflammation rather than a malignancy. The patient's symptoms, including dysphagia and it was improved remarkably after endoscopic mucosal resection (EMR). The EMR indicated that the lesion was benign. A follow-up endoscopy three months later showed no signs of the lesion, and histopathology confirmed that it was benign inflammation with no evidence of cancer.

Disclosures:
Ahmad Sandouka, 1, Sayed T. Shah, 2, Mohammed W Khaled, MD3, Barakat Aburajab Altamimi, MD4. P2269 - From Dysphagia to Diagnosis: An Esophageal Enigma in a Post-Bacteremia Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nicosia St. George's Medical School, Nicosia, Nicosia, Cyprus; 2University of Nicosia Medical School, Abbotsford, BC, Canada; 3King Hussein Medical Center, Amman, 'Amman, Jordan; 4Mercy Medical Center, Cedar Rapids, IA
Introduction: Esophageal abscess is a condition, when there is a buildup of pus within the esophagus. Severe chest discomfort, fever, and trouble swallowing are symptoms of esophageal abscesses. This can be caused by trauma, infections, or perforations. To avoid further complications like sepsis and mediastinitis, It can be diagnosed by imaging and treatment with antibiotics as well as drainage is critical.
Case Description/Methods: A 59-year-old male, who had Lyme disease and asthma visited the ER with painful dysphagia. A month prior, he had received treatment for bacteremia, likely related to dental issues. Antibiotics initially helped to improve his condition, but a few days prior to his latest ER visit, he experienced a recurrence of his symptoms, which included significant chest pressure and recurrent hiccups. Mildly enlarged mediastinal and left hilar lymph nodes were discovered on a prior CT scan of the chest. The patient went back to the ER and complained of losing five pounds since his last hospital admission, difficulty swallowing, and the feeling that food was lodged in his esophagus. Abdominal pain, chills, nausea, vomiting, diarrhea, fever, and night sweats were all denied by him. The over-the-counter antacids did not work. Through an esophagogastroduodenoscopy (EGD) a mid-esophageal lesion was discovered. An endoscopic ultrasonography (EUS) detected a sizable hypoechoic lymph node (22 mm by 14 mm) in station 4L. With shadowing foci, the esophageal lesion at 30 cm from the incisura seemed superficial to the muscularis propria. There was no abnormal lymphadenopathy in the areas. An abscess was discovered during an endoscopic mucosal resection (EMR), which revealed purulent material from the lesion. After his lesion was removed, later a biopsy of the base revealed no perforation. Pathology confirmed that the lymph node did not contain any cancer cells and that there was benign squamous mucosa with acute, chronic, and granulomatous inflammation. Following the EMR, the patient's symptoms were resolved. An EGD three months later revealed no residual lesion.
Discussion: In this case, the presence of purulent material depicted an infectious or inflammation rather than a malignancy. The patient's symptoms, including dysphagia and it was improved remarkably after endoscopic mucosal resection (EMR). The EMR indicated that the lesion was benign. A follow-up endoscopy three months later showed no signs of the lesion, and histopathology confirmed that it was benign inflammation with no evidence of cancer.

Figure: mid esophageal lesion noted on upper endoscopy
Disclosures:
Ahmad Sandouka indicated no relevant financial relationships.
Sayed Shah indicated no relevant financial relationships.
Mohammed W Khaled indicated no relevant financial relationships.
Barakat Aburajab Altamimi indicated no relevant financial relationships.
Ahmad Sandouka, 1, Sayed T. Shah, 2, Mohammed W Khaled, MD3, Barakat Aburajab Altamimi, MD4. P2269 - From Dysphagia to Diagnosis: An Esophageal Enigma in a Post-Bacteremia Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
