Monday Poster Session
Category: Esophagus
P2277 - A Rare Case of Esophageal Squamous Cell Carcinoma Arising From Barrett’s Segment With High Grade Dysplasia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MP
Madison B. Peregoy, MD
National Capital Consortium
Bethesda, MD
Presenting Author(s)
Madison B. Peregoy, MD1, Chelsea Forbes, MD2, Patrick E. Young, MD, FACG2
1National Capital Consortium, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Barrett’s esophagus (BE) is the only known precursor lesion to esophageal adenocarcinoma (EAC). While there are some overlapping risk factors for the development of BE and Esophageal Squamous Cell Carcinoma (ESCC), BE is not considered a precursor to ESCC. We describe a rare case of ESCC arising from a segment of BE with high-grade dysplasia, which presents unique diagnostic and therapeutic challenges.
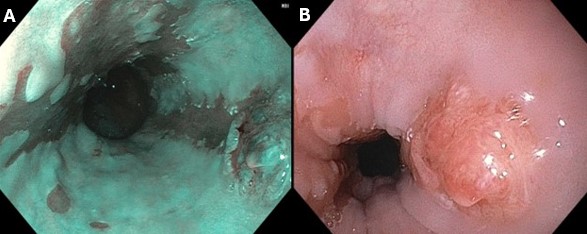
Case Description/Methods: A 65-year-old male with a history of BE, recurrent alcohol-associated pancreatitis, tobacco use, lung disease, and iron deficiency anemia (IDA) was hospitalized for worsening anemia suggestive of occult gastrointestinal bleeding. During this admission, an EGD was performed, which demonstrated long-segment BE (C2M5) and a nodular lesion at the proximal extent of the longest Barrett’s tongue. He was referred for repeat endoscopy with band-assisted endoscopic mucosal resection (EMR) of the nodular lesion shown in Figure 1. The remainder of the BE segment was biopsied per Seattle protocol. Histopathologic examination of the EMR specimen showed moderately-differentiated invasive ESCC (T1b with lymphovascular invasion) in a background of intestinal metaplasia. Margins of the EMR specimen were negative for tumor, and no obvious metastatic disease was found on PET scan. Biopsies taken from adjacent tissue in the BE segment showed high-grade dysplasia. He was deemed a poor surgical candidate and recommended to undergo adjuvant chemoradiation and ablation of the Barrett’s esophagus.
Discussion: Endoscopic surveillance for BE aims to detect neoplasia at an early stage to avoid the morbidity and mortality associated with the treatment of advanced EAC. This case underscores the necessity of endoscopic resection (ER) for visible BE lesions prior to ablative techniques as part of endoscopic eradication therapy (EET). While recent studies suggest that EAC with superficial submucosal invasion (T1b) and favorable histology may be adequately treated with EET alone, ESCC carries a higher risk of nodal metastasis. Therefore, adjuvant chemoradiation therapy, or potentially esophagectomy if patient is a surgical candidate, should be considered in addition to EET for treatment of remaining dysplastic BE. Given the rarity of this case, further research is needed to understand the pathophysiological mechanism and identify risk factors driving malignant transformation of BE to ESCC.
Disclosures:
Madison B. Peregoy, MD1, Chelsea Forbes, MD2, Patrick E. Young, MD, FACG2. P2277 - A Rare Case of Esophageal Squamous Cell Carcinoma Arising From Barrett’s Segment With High Grade Dysplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1National Capital Consortium, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Barrett’s esophagus (BE) is the only known precursor lesion to esophageal adenocarcinoma (EAC). While there are some overlapping risk factors for the development of BE and Esophageal Squamous Cell Carcinoma (ESCC), BE is not considered a precursor to ESCC. We describe a rare case of ESCC arising from a segment of BE with high-grade dysplasia, which presents unique diagnostic and therapeutic challenges.
Case Description/Methods: A 65-year-old male with a history of BE, recurrent alcohol-associated pancreatitis, tobacco use, lung disease, and iron deficiency anemia (IDA) was hospitalized for worsening anemia suggestive of occult gastrointestinal bleeding. During this admission, an EGD was performed, which demonstrated long-segment BE (C2M5) and a nodular lesion at the proximal extent of the longest Barrett’s tongue. He was referred for repeat endoscopy with band-assisted endoscopic mucosal resection (EMR) of the nodular lesion shown in Figure 1. The remainder of the BE segment was biopsied per Seattle protocol. Histopathologic examination of the EMR specimen showed moderately-differentiated invasive ESCC (T1b with lymphovascular invasion) in a background of intestinal metaplasia. Margins of the EMR specimen were negative for tumor, and no obvious metastatic disease was found on PET scan. Biopsies taken from adjacent tissue in the BE segment showed high-grade dysplasia. He was deemed a poor surgical candidate and recommended to undergo adjuvant chemoradiation and ablation of the Barrett’s esophagus.
Discussion: Endoscopic surveillance for BE aims to detect neoplasia at an early stage to avoid the morbidity and mortality associated with the treatment of advanced EAC. This case underscores the necessity of endoscopic resection (ER) for visible BE lesions prior to ablative techniques as part of endoscopic eradication therapy (EET). While recent studies suggest that EAC with superficial submucosal invasion (T1b) and favorable histology may be adequately treated with EET alone, ESCC carries a higher risk of nodal metastasis. Therefore, adjuvant chemoradiation therapy, or potentially esophagectomy if patient is a surgical candidate, should be considered in addition to EET for treatment of remaining dysplastic BE. Given the rarity of this case, further research is needed to understand the pathophysiological mechanism and identify risk factors driving malignant transformation of BE to ESCC.
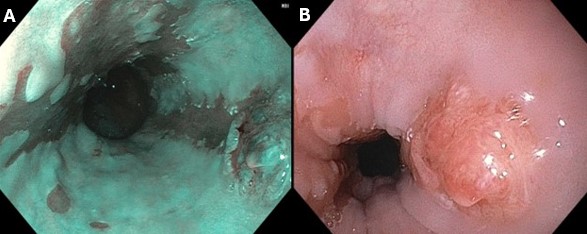
Figure: Figure 1: A) Barrett's Esophagus (C5M7), B) 1cm nodular lesion at the distal extent of Barrett’s tongue with abnormal mucosa and overlying telangiectasia.
Disclosures:
Madison Peregoy indicated no relevant financial relationships.
Chelsea Forbes indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Madison B. Peregoy, MD1, Chelsea Forbes, MD2, Patrick E. Young, MD, FACG2. P2277 - A Rare Case of Esophageal Squamous Cell Carcinoma Arising From Barrett’s Segment With High Grade Dysplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

