Monday Poster Session
Category: Esophagus
P2284 - Nondiabetic Gastric Outlet Obstruction With Duodenal Ulcer Leading to Acute Esophageal Necrosis in 88-Year-Old Male
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BB
Brennan Bohman, DO
United States Air Force
Biloxi, MS
Presenting Author(s)
Brennan Bohman, DO, Devlin Farr, DO, David Shumway, DO, Wassem Juakiem, MS, MD
United States Air Force, Biloxi, MS
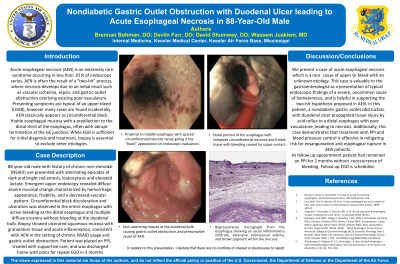
Introduction: Acute esophageal necrosis (AEN) is an extremely rare syndrome occurring in less than .01% of endoscopy series. AEN is often the result of a “two-hit” process, where necrosis develops due to an initial insult such as vascular ischemia, sepsis, and gastric outlet obstruction overlying existing poor vasculature. Presenting symptoms are typical of an upper bleed (UGIB), with melena and hematemesis, however many cases are found incidentally. On upper endoscopy (EGD), AEN classically appears as circumferential black friable esophageal mucosa with a predilection to the distal third of the esophagus, often with abrupt termination at the GE junction. While EGD is sufficient for initial diagnosis and treatment, biopsy is essential to exclude other etiologies.
Case Description/Methods: 88-year-old male with history of chronic non-steroidal (NSAID) use presented with alternating episodes of dark and bright red emesis, leukocytosis and elevated lactate. Emergent upper endoscopy revealed diffuse severe mucosal change characterized by hemorrhagic appearance, friability, and a decreased vascular pattern. Circumferential black discoloration and ulceration was observed in the entire esophagus with active bleeding at the distal esophagus and multiple diffuse erosions without bleeding at the duodenal bulb. Biopsy showed ulcerated squamous mucosa with granulation tissue and acute inflammation, consistent with AEN in the setting of chronic NSAID usage and gastric outlet obstruction. Patient was placed on PPI, treated with supportive care, and was discharged home with plans for repeat EGD in 3 months.
Discussion: Our case is valuable to the gastroenterologist as a presentation of typical endoscopic findings of a severe, uncommon cause of hematemesis, and is helpful in supporting the two-hit hypothesis proposed in AEN. In this patient, a nondiabetic gastric outlet obstruction with duodenal ulcer propagated tissue injury by acid reflux to a distal esophagus with poor vasculature, leading to necrosis. Additionally, this case demonstrates that treatment with PPI and blood pressure control is effective in mitigating risk for exsanguination and esophageal rupture in AEN patients.
Disclosures:
Brennan Bohman, DO, Devlin Farr, DO, David Shumway, DO, Wassem Juakiem, MS, MD. P2284 - Nondiabetic Gastric Outlet Obstruction With Duodenal Ulcer Leading to Acute Esophageal Necrosis in 88-Year-Old Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
United States Air Force, Biloxi, MS
Introduction: Acute esophageal necrosis (AEN) is an extremely rare syndrome occurring in less than .01% of endoscopy series. AEN is often the result of a “two-hit” process, where necrosis develops due to an initial insult such as vascular ischemia, sepsis, and gastric outlet obstruction overlying existing poor vasculature. Presenting symptoms are typical of an upper bleed (UGIB), with melena and hematemesis, however many cases are found incidentally. On upper endoscopy (EGD), AEN classically appears as circumferential black friable esophageal mucosa with a predilection to the distal third of the esophagus, often with abrupt termination at the GE junction. While EGD is sufficient for initial diagnosis and treatment, biopsy is essential to exclude other etiologies.
Case Description/Methods: 88-year-old male with history of chronic non-steroidal (NSAID) use presented with alternating episodes of dark and bright red emesis, leukocytosis and elevated lactate. Emergent upper endoscopy revealed diffuse severe mucosal change characterized by hemorrhagic appearance, friability, and a decreased vascular pattern. Circumferential black discoloration and ulceration was observed in the entire esophagus with active bleeding at the distal esophagus and multiple diffuse erosions without bleeding at the duodenal bulb. Biopsy showed ulcerated squamous mucosa with granulation tissue and acute inflammation, consistent with AEN in the setting of chronic NSAID usage and gastric outlet obstruction. Patient was placed on PPI, treated with supportive care, and was discharged home with plans for repeat EGD in 3 months.
Discussion: Our case is valuable to the gastroenterologist as a presentation of typical endoscopic findings of a severe, uncommon cause of hematemesis, and is helpful in supporting the two-hit hypothesis proposed in AEN. In this patient, a nondiabetic gastric outlet obstruction with duodenal ulcer propagated tissue injury by acid reflux to a distal esophagus with poor vasculature, leading to necrosis. Additionally, this case demonstrates that treatment with PPI and blood pressure control is effective in mitigating risk for exsanguination and esophageal rupture in AEN patients.
Disclosures:
Brennan Bohman indicated no relevant financial relationships.
Devlin Farr indicated no relevant financial relationships.
David Shumway indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Brennan Bohman, DO, Devlin Farr, DO, David Shumway, DO, Wassem Juakiem, MS, MD. P2284 - Nondiabetic Gastric Outlet Obstruction With Duodenal Ulcer Leading to Acute Esophageal Necrosis in 88-Year-Old Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
