Monday Poster Session
Category: Esophagus
P2285 - Heterotopic Pancreatic Tissue at the Gastroesophageal Junction Mimicking Barrett’s Esophagus
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Raza Muhammad, DO
University of Chicago Northshore
Chicago, IL
Presenting Author(s)
Raza Muhammad, DO1, Sarah Burroughs, DO2, David Weinstein, MD3, Robert Toelke, MD4, Farhan Quader, MD4
1University of Chicago Northshore, Evanston, IL; 2University of Chicago, Northshore University Healthsystem, Evanston, IL; 3University of Chicago, NorthShore Internal Medicine, Evanston, IL; 4NorthShore University HealthSystem, Evanston, IL
Introduction: Heterotopic pancreatic tissue is defined as extrapancreatic tissue without vascular or anatomic connection to the pancreas. We present a rare case of heterotopic pancreatic tissue found at the gastroesophageal junction (GEJ) that was endoscopically indistinguishable from short-segment Barrett’s Esophagus.
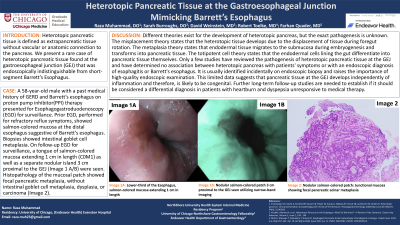
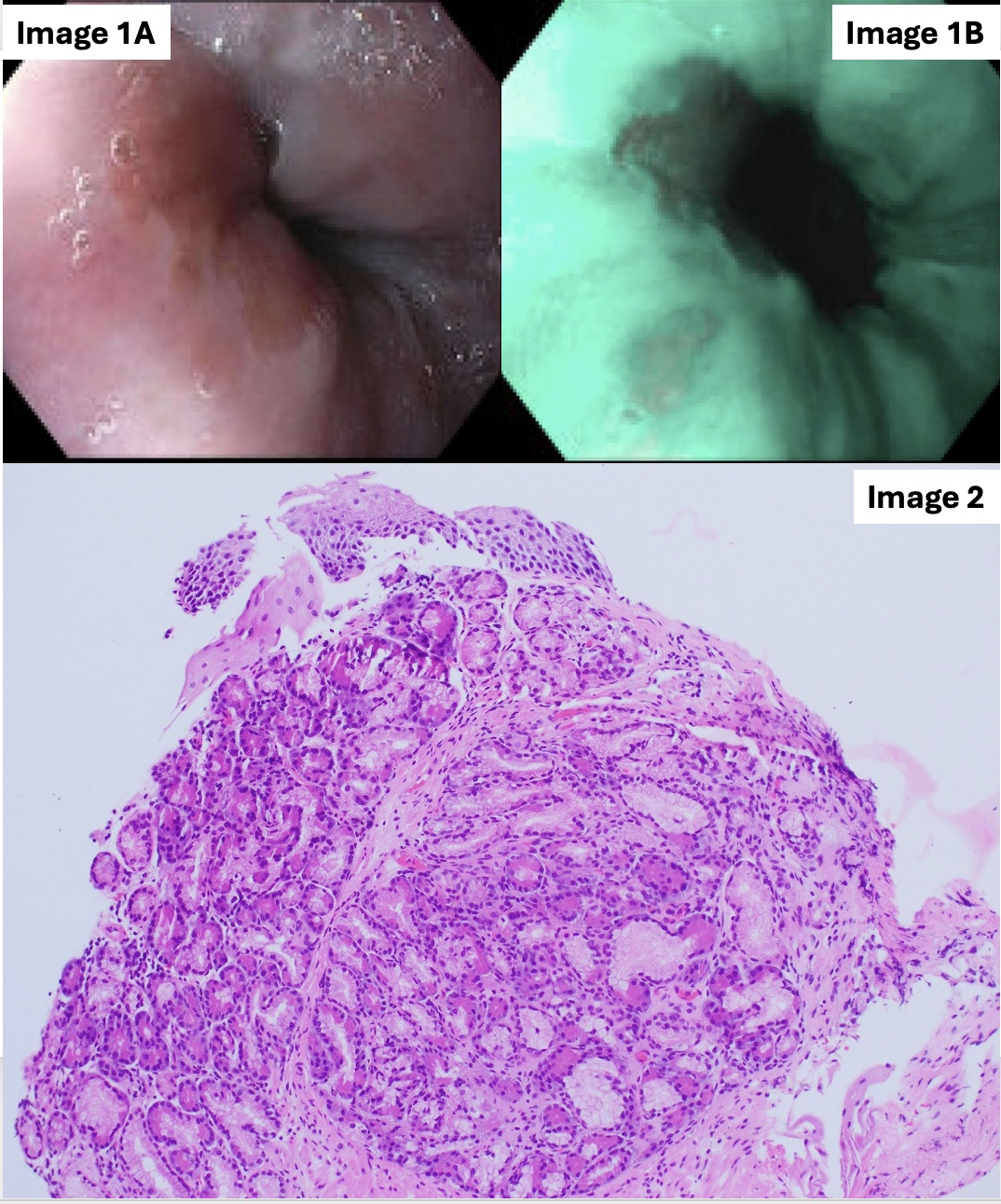
Case Description/Methods: A 58-year-old male with past medical history of GERD and Barrett’s esophagus on proton pump inhibitor (PPI) therapy presented for Esophagogastroduodenoscopy (EGD) for surveillance. Prior EGD, performed for refractory reflux symptoms, showed salmon-colored mucosa at the distal esophagus suggestive of Barrett’s esophagus. Biopsies showed intestinal goblet cell metaplasia. On follow-up EGD for surveillance, a tongue of salmon-colored mucosa extending 1 cm in length (C0M1) as well as a separate nodular island 3 cm proximal to the GEJ (Image 1 A/B) were seen. Histopathology of the mucosal patch showed focal pancreatic metaplasia, without intestinal goblet cell metaplasia, dysplasia, or carcinoma (Image 2).
Discussion: Different theories exist for the development of heterotopic pancreas, but the exact pathogenesis is unknown. The misplacement theory states that the heterotopic tissue develops due to the displacement of tissue during foregut rotation. The metaplasia theory states that endodermal tissue migrates to the submucosa during embryogenesis and transforms into pancreatic tissue. The totipotent cell theory states that the endodermal cells lining the gut differentiate into pancreatic tissue themselves. Only a few studies have reviewed the pathogenesis of heterotopic pancreatic tissue at the GEJ and have determined no association between heterotopic pancreas with patients' symptoms or with an endoscopic diagnosis of esophagitis or Barrett's esophagus. It is usually identified incidentally on endoscopic biopsy, and raises the importance of high-quality endoscopic examination. This limited data suggests that pancreatic tissue at the GEJ develops independently of inflammation and therefore, is likely to be congenital. Further long-term follow-up studies are needed to establish if it should be considered a differential diagnosis in patients with heartburn and dyspepsia unresponsive to medical therapy.
Disclosures:
Raza Muhammad, DO1, Sarah Burroughs, DO2, David Weinstein, MD3, Robert Toelke, MD4, Farhan Quader, MD4. P2285 - Heterotopic Pancreatic Tissue at the Gastroesophageal Junction Mimicking Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago Northshore, Evanston, IL; 2University of Chicago, Northshore University Healthsystem, Evanston, IL; 3University of Chicago, NorthShore Internal Medicine, Evanston, IL; 4NorthShore University HealthSystem, Evanston, IL
Introduction: Heterotopic pancreatic tissue is defined as extrapancreatic tissue without vascular or anatomic connection to the pancreas. We present a rare case of heterotopic pancreatic tissue found at the gastroesophageal junction (GEJ) that was endoscopically indistinguishable from short-segment Barrett’s Esophagus.
Case Description/Methods: A 58-year-old male with past medical history of GERD and Barrett’s esophagus on proton pump inhibitor (PPI) therapy presented for Esophagogastroduodenoscopy (EGD) for surveillance. Prior EGD, performed for refractory reflux symptoms, showed salmon-colored mucosa at the distal esophagus suggestive of Barrett’s esophagus. Biopsies showed intestinal goblet cell metaplasia. On follow-up EGD for surveillance, a tongue of salmon-colored mucosa extending 1 cm in length (C0M1) as well as a separate nodular island 3 cm proximal to the GEJ (Image 1 A/B) were seen. Histopathology of the mucosal patch showed focal pancreatic metaplasia, without intestinal goblet cell metaplasia, dysplasia, or carcinoma (Image 2).
Discussion: Different theories exist for the development of heterotopic pancreas, but the exact pathogenesis is unknown. The misplacement theory states that the heterotopic tissue develops due to the displacement of tissue during foregut rotation. The metaplasia theory states that endodermal tissue migrates to the submucosa during embryogenesis and transforms into pancreatic tissue. The totipotent cell theory states that the endodermal cells lining the gut differentiate into pancreatic tissue themselves. Only a few studies have reviewed the pathogenesis of heterotopic pancreatic tissue at the GEJ and have determined no association between heterotopic pancreas with patients' symptoms or with an endoscopic diagnosis of esophagitis or Barrett's esophagus. It is usually identified incidentally on endoscopic biopsy, and raises the importance of high-quality endoscopic examination. This limited data suggests that pancreatic tissue at the GEJ develops independently of inflammation and therefore, is likely to be congenital. Further long-term follow-up studies are needed to establish if it should be considered a differential diagnosis in patients with heartburn and dyspepsia unresponsive to medical therapy.
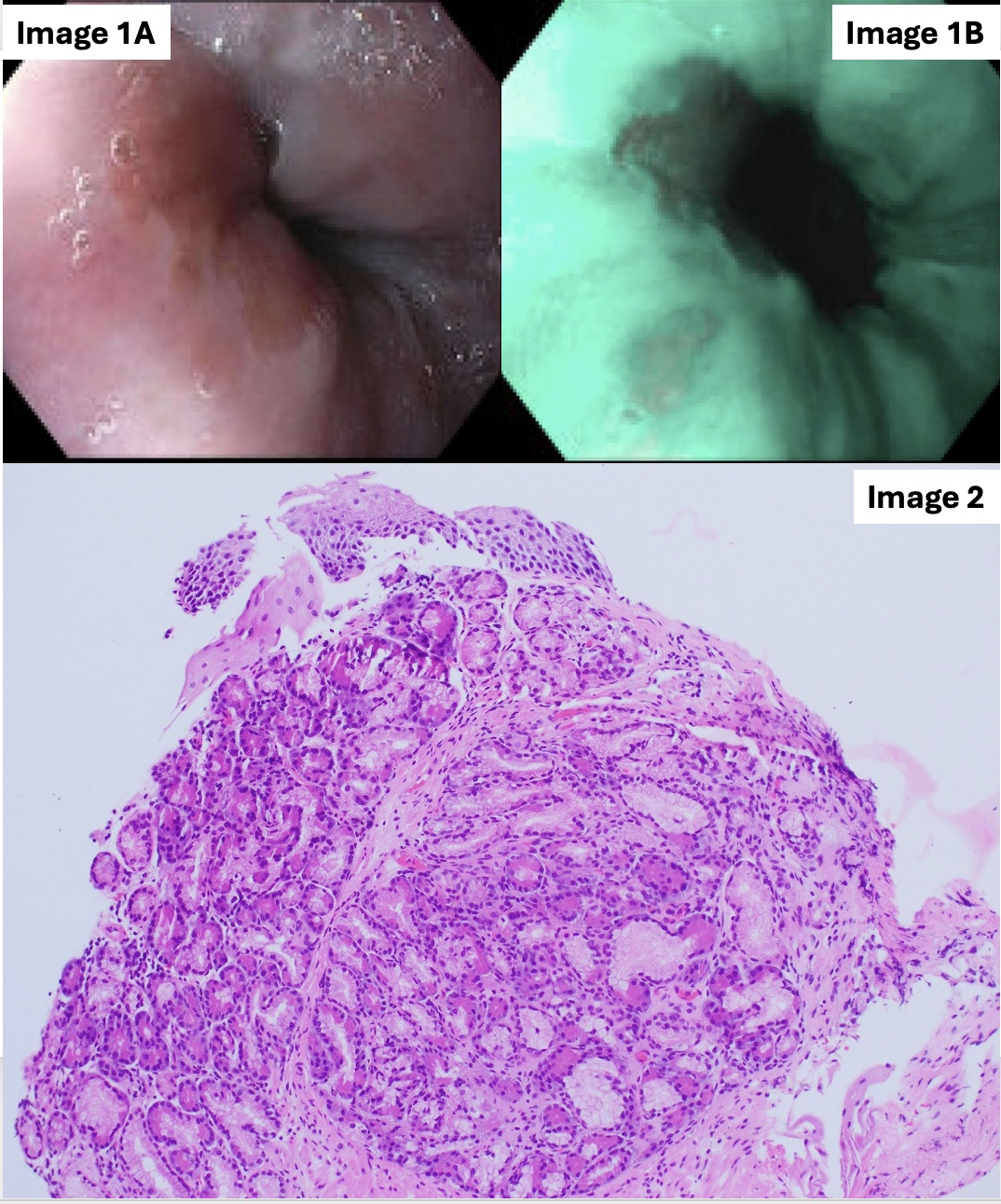
Figure: Image 1: Lower-third of the esophagus (1A): Salmon-colored mucosa extending 1 cm in length (1B): Nodular salmon-colored patch 3 cm proximal to the GEJ seen utilizing narrow-band imaging
Image 2: Nodular salmon-colored patch: Junctional mucosa showing focal pancreatic acinar metaplasia
Image 2: Nodular salmon-colored patch: Junctional mucosa showing focal pancreatic acinar metaplasia
Disclosures:
Raza Muhammad indicated no relevant financial relationships.
Sarah Burroughs indicated no relevant financial relationships.
David Weinstein indicated no relevant financial relationships.
Robert Toelke indicated no relevant financial relationships.
Farhan Quader: Castle Biosciences – Advisory Committee/Board Member, Speakers Bureau.
Raza Muhammad, DO1, Sarah Burroughs, DO2, David Weinstein, MD3, Robert Toelke, MD4, Farhan Quader, MD4. P2285 - Heterotopic Pancreatic Tissue at the Gastroesophageal Junction Mimicking Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
