Monday Poster Session
Category: Esophagus
P2296 - Difficult to Stomach: A Case of Esophagopleural Fistula Complicated by Stent Migration
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Charles B. Woodall, DO
Louisiana State University Health Sciences Center
Covington, LA
Presenting Author(s)
Charles B. Woodall, DO1, Nikki Arceneaux, MD2
1Louisiana State University Health Sciences Center, Covington, LA; 2Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Esophagopleural fistula (EPF) is a rare occurrence that generally forms secondary to infection, malignancy, instrumentation, or surgery. Spontaneous EPF occurs even less frequently and only a limited number of cases are documented in the literature. All EPFs are associated with significant morbidity and mortality making early recognition and intervention essential.
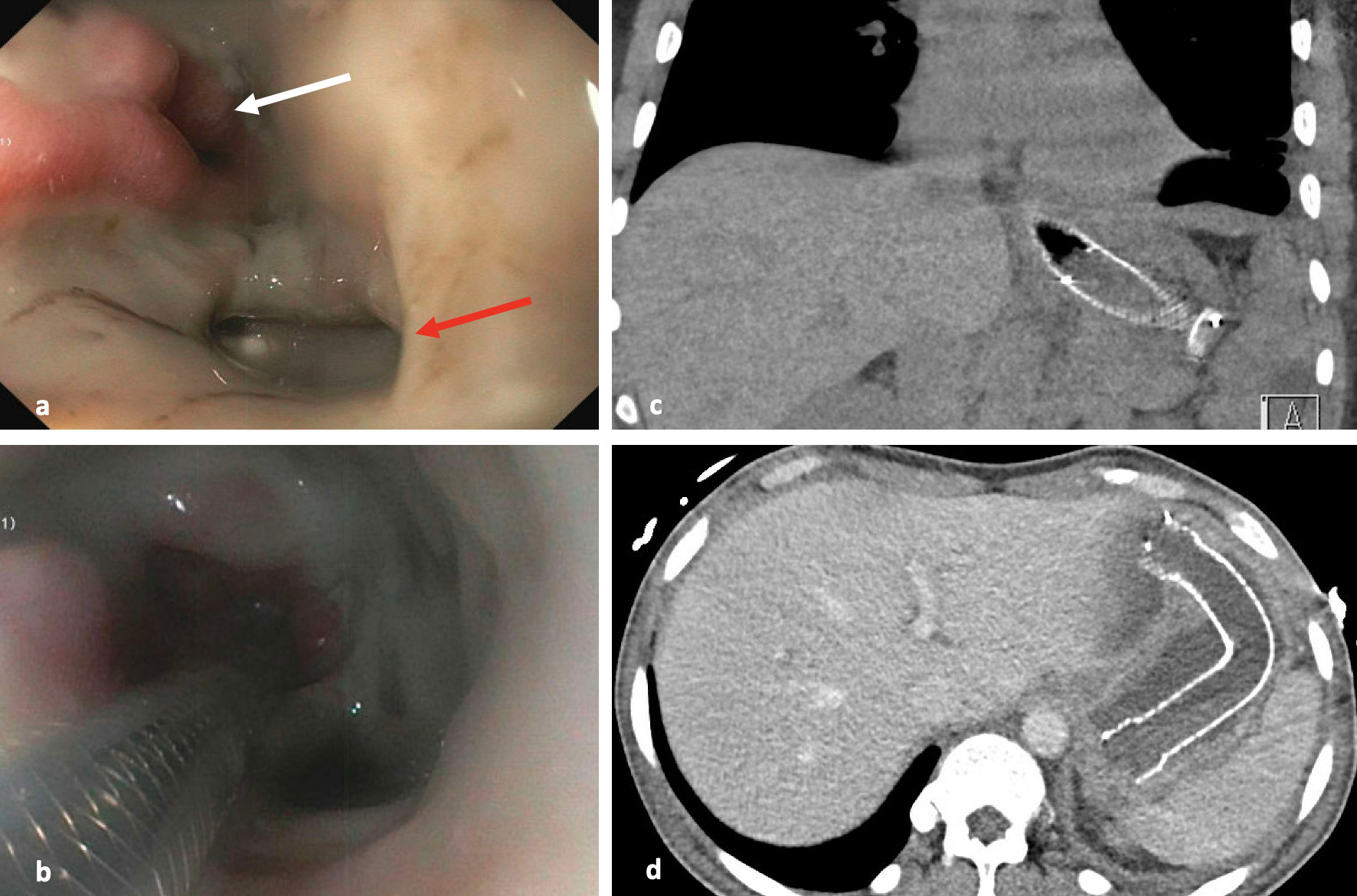
Case Description/Methods: A 53-year-old male with a history of esophagitis with stricture, gastroparesis, and diabetes mellitus initially presented with complaints of left-sided chest pain that woke him from sleep. Broad spectrum antibiotics were started given his worsening encephalopathy, and imaging revealed a pleural effusion. A chest tube was placed that confirmed empyema, and an esophagopleural fistula was discovered shortly thereafter when oral vitamin K was seen draining from the chest tube. EGD revealed a 2.5 cm fistula through which the chest tube could be visualized and LA grade D esophagitis. A covered metallic stent was placed and secured with a clip, and a jejunostomy tube was placed for nutrition and medication administration. PPI therapy was continued, and stent removal/revision was planned for eight weeks later. Unfortunately, the patient was lost to follow up until presenting three months later with additional complaints of left-sided chest pain and was found to have a recurrent pleural effusion. No redemonstration of the EPF was present, but significant esophagitis and stenosis as well as partial stent migration into the stomach was appreciated. Outpatient stent removal was again planned upon discharge, but the patient was lost to follow up once more before returning five months later with complaint of persistent vomiting following oral intake for one month. Complete stent migration into the stomach was evident on imaging. Stent removal was deferred during EGD due to recurrent esophagitis and stenosis. Future outpatient GI follow up is currently pending.
Discussion: Spontaneous EPF is an extremely rare condition with an overall poor prognosis. Early diagnosis and intervention are critical. Diagnosis is typically made via chest imaging with CT demonstrating particular utility. Management varies depends on location, severity, and duration of the EPF. Conservative measures include empyema drainage and irrigation with enteral feeding. Endoscopic repair can be attempted with clipping or stenting with the understanding that stent migration is not an uncommon complication, or surgical intervention can be considered.
Disclosures:
Charles B. Woodall, DO1, Nikki Arceneaux, MD2. P2296 - Difficult to Stomach: A Case of Esophagopleural Fistula Complicated by Stent Migration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Louisiana State University Health Sciences Center, Covington, LA; 2Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Esophagopleural fistula (EPF) is a rare occurrence that generally forms secondary to infection, malignancy, instrumentation, or surgery. Spontaneous EPF occurs even less frequently and only a limited number of cases are documented in the literature. All EPFs are associated with significant morbidity and mortality making early recognition and intervention essential.
Case Description/Methods: A 53-year-old male with a history of esophagitis with stricture, gastroparesis, and diabetes mellitus initially presented with complaints of left-sided chest pain that woke him from sleep. Broad spectrum antibiotics were started given his worsening encephalopathy, and imaging revealed a pleural effusion. A chest tube was placed that confirmed empyema, and an esophagopleural fistula was discovered shortly thereafter when oral vitamin K was seen draining from the chest tube. EGD revealed a 2.5 cm fistula through which the chest tube could be visualized and LA grade D esophagitis. A covered metallic stent was placed and secured with a clip, and a jejunostomy tube was placed for nutrition and medication administration. PPI therapy was continued, and stent removal/revision was planned for eight weeks later. Unfortunately, the patient was lost to follow up until presenting three months later with additional complaints of left-sided chest pain and was found to have a recurrent pleural effusion. No redemonstration of the EPF was present, but significant esophagitis and stenosis as well as partial stent migration into the stomach was appreciated. Outpatient stent removal was again planned upon discharge, but the patient was lost to follow up once more before returning five months later with complaint of persistent vomiting following oral intake for one month. Complete stent migration into the stomach was evident on imaging. Stent removal was deferred during EGD due to recurrent esophagitis and stenosis. Future outpatient GI follow up is currently pending.
Discussion: Spontaneous EPF is an extremely rare condition with an overall poor prognosis. Early diagnosis and intervention are critical. Diagnosis is typically made via chest imaging with CT demonstrating particular utility. Management varies depends on location, severity, and duration of the EPF. Conservative measures include empyema drainage and irrigation with enteral feeding. Endoscopic repair can be attempted with clipping or stenting with the understanding that stent migration is not an uncommon complication, or surgical intervention can be considered.
Figure: a. Esophagopleural fistula (red arrow) can be seen just proximal to the lower esophageal sphincter (white arrow) ; b. Covered metallic stent can be seen traversing the esophagopleural fistula prior to deployment; c. CT imaging demonstrating partial migration of stent into the stomach; d. Subsequent CT imaging demonstrating complete migration of the esophageal stent into the patient's stomach during most recent admission
Disclosures:
Charles Woodall indicated no relevant financial relationships.
Nikki Arceneaux indicated no relevant financial relationships.
Charles B. Woodall, DO1, Nikki Arceneaux, MD2. P2296 - Difficult to Stomach: A Case of Esophagopleural Fistula Complicated by Stent Migration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
