Monday Poster Session
Category: Esophagus
P2297 - Russell Body Esophagitis Without Associated Barrett’s Esophagus: One of Two Reported Cases
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Charlie Altfillisch, MD
University of Kansas Medical Center
Kansas City, MO
Presenting Author(s)
Award: Presidential Poster Award
Charles Altfillisch, MD1, Pranay Reddy, MD, MPH2, Salih Samo, MD, MS2
1University of Kansas Medical Center, Kansas City, MO; 2University of Kansas Medical Center, Kansas City, KS
Introduction: Russell body esophagitis (RBE) is rarely reported in medical literature, with only six documented cases, one of which was not associated with Barrett’s esophagus. This pathology is often linked to chronic inflammatory processes and is characterized by eosinophilic, immunoglobin-containing plasma cell inclusions (Russell bodies), most commonly in the gastric antrum. An association with H. pylori has also been documented. This case highlights the second reported instance of RBE in a patient without H. pylori and Barrett’s esophagus.
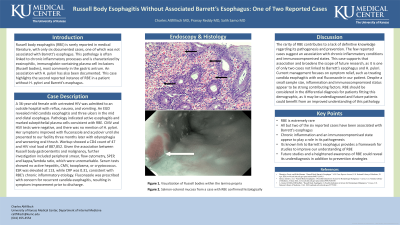
Case Description/Methods: A 36-year-old female with untreated HIV was admitted to an outside hospital with reflux, nausea, and vomiting. An EGD revealed mild candida esophagitis and three ulcers in the mid and distal esophagus. Pathology indicated active esophagitis with marked subepithelial plasma cells consistent with RBE. CMV and HSV tests were negative, and there was no mention of H. pylori infection. Her symptoms improved with fluconazole and acyclovir until she presented to our facility three months later with odynophagia and worsening oral thrush. Workup showed a CD4 count of 47 and HIV viral load of 887,852. Given the association between Russell body gastroenteritis and malignancy, further investigation was pursued including peripheral smear, peripheral flow cytometry, SPEP, and kappa/lambda ratio, which was unremarkable. Serum tests showed no active hepatitis, CMV, toxoplasma, or cryptococcus. ESR was elevated at 113, while CRP was 0.31, consistent with RBE’s chronic inflammatory etiology. Due to her history and concern for recurrent candida esophagitis, she was treated again with fluconazole, resulting in symptom improvement prior to discharge.
Discussion: The rarity of RBE contributes to a lack of definitive knowledge regarding its pathogenesis and prevention. The few reported cases suggest an association with chronic inflammatory conditions and immunocompromised states. This case supports that association and broadens the scope of future research, as it is one of only two cases not linked to Barrett’s esophagus and H. pylori. Current management focuses on symptom relief, such as treating candida esophagitis with oral fluconazole in our patient. Despite a small sample size, inflammation and immunocompromised status appear to be strong contributing factors. RBE should be considered in the differential diagnosis for patients fitting this demographic, as it may be underdiagnosed and future patients could benefit from an improved understanding of this pathology.
Disclosures:
Charles Altfillisch, MD1, Pranay Reddy, MD, MPH2, Salih Samo, MD, MS2. P2297 - Russell Body Esophagitis Without Associated Barrett’s Esophagus: One of Two Reported Cases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Charles Altfillisch, MD1, Pranay Reddy, MD, MPH2, Salih Samo, MD, MS2
1University of Kansas Medical Center, Kansas City, MO; 2University of Kansas Medical Center, Kansas City, KS
Introduction: Russell body esophagitis (RBE) is rarely reported in medical literature, with only six documented cases, one of which was not associated with Barrett’s esophagus. This pathology is often linked to chronic inflammatory processes and is characterized by eosinophilic, immunoglobin-containing plasma cell inclusions (Russell bodies), most commonly in the gastric antrum. An association with H. pylori has also been documented. This case highlights the second reported instance of RBE in a patient without H. pylori and Barrett’s esophagus.
Case Description/Methods: A 36-year-old female with untreated HIV was admitted to an outside hospital with reflux, nausea, and vomiting. An EGD revealed mild candida esophagitis and three ulcers in the mid and distal esophagus. Pathology indicated active esophagitis with marked subepithelial plasma cells consistent with RBE. CMV and HSV tests were negative, and there was no mention of H. pylori infection. Her symptoms improved with fluconazole and acyclovir until she presented to our facility three months later with odynophagia and worsening oral thrush. Workup showed a CD4 count of 47 and HIV viral load of 887,852. Given the association between Russell body gastroenteritis and malignancy, further investigation was pursued including peripheral smear, peripheral flow cytometry, SPEP, and kappa/lambda ratio, which was unremarkable. Serum tests showed no active hepatitis, CMV, toxoplasma, or cryptococcus. ESR was elevated at 113, while CRP was 0.31, consistent with RBE’s chronic inflammatory etiology. Due to her history and concern for recurrent candida esophagitis, she was treated again with fluconazole, resulting in symptom improvement prior to discharge.
Discussion: The rarity of RBE contributes to a lack of definitive knowledge regarding its pathogenesis and prevention. The few reported cases suggest an association with chronic inflammatory conditions and immunocompromised states. This case supports that association and broadens the scope of future research, as it is one of only two cases not linked to Barrett’s esophagus and H. pylori. Current management focuses on symptom relief, such as treating candida esophagitis with oral fluconazole in our patient. Despite a small sample size, inflammation and immunocompromised status appear to be strong contributing factors. RBE should be considered in the differential diagnosis for patients fitting this demographic, as it may be underdiagnosed and future patients could benefit from an improved understanding of this pathology.
Disclosures:
Charles Altfillisch indicated no relevant financial relationships.
Pranay Reddy indicated no relevant financial relationships.
Salih Samo: Castle Biosciences – Advisory Committee/Board Member, Consultant, Speakers Bureau. EndoGastric Solutions – Speakers Bureau. Evoke – Speakers Bureau. Medtronic – Speakers Bureau. Phathom – Speakers Bureau. Sanofi – Advisory Committee/Board Member, Consultant.
Charles Altfillisch, MD1, Pranay Reddy, MD, MPH2, Salih Samo, MD, MS2. P2297 - Russell Body Esophagitis Without Associated Barrett’s Esophagus: One of Two Reported Cases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

