Monday Poster Session
Category: Esophagus
P2300 - Acute Esophageal Necrosis: An Uncommon Culprit Behind Upper GI Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jose W. Sotelo, MD
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Jose W. Sotelo, MD1, Akanksha Togra, MD1, John Joyce, MD2, Brian Lee, DO3, Pratyusha TIrumanisetty, MD4
1Texas Tech University Health Sciences Center, El Paso, TX; 2SUNY Upstate Medical University, Syracuse, NY; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, San Antonio, TX; 4Memorial Medical Center, El Paso, TX
Introduction: Acute esophageal necrosis (AEN), or "black esophagus," is a rare, serious condition marked by widespread necrosis of the esophageal mucosa. It often presents with upper gastrointestinal bleeding, sepsis, or signs of peripheral hypoperfusion, mainly affecting elderly patients with comorbidities like diabetes, cardiovascular disease, and chronic renal insufficiency. This report details the case of an 80-year-old female with poorly controlled diabetes who developed AEN during septic shock from emphysematous pyelonephritis.
Case Description/Methods: An 80-year-old female with poorly controlled diabetes presented to the Emergency Department in septic shock due to emphysematous pyelonephritis. Admitted to the ICU, she was treated with vasopressors and antibiotics. On the fourth day, she developed coffee-ground emesis and melena, with hemoglobin dropping from 12 g/dL to 7 g/dL. Despite this, she was hemodynamically stable and started on a proton pump inhibitor (PPI).
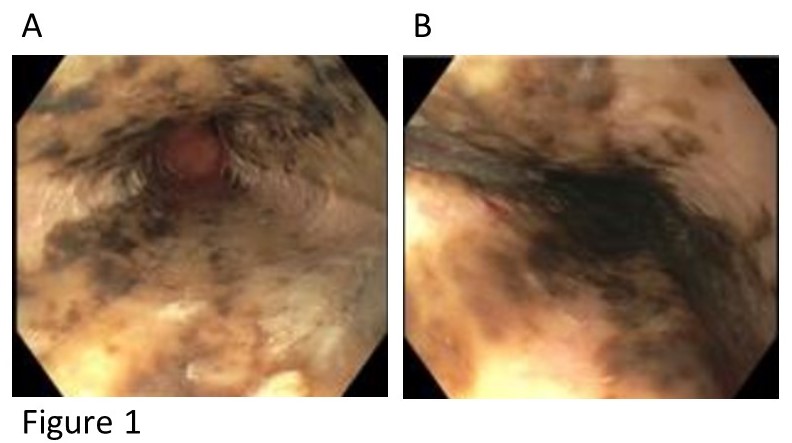
An esophagogastroduodenoscopy (EGD) showed diffuse esophageal necrosis sparing the gastroesophageal junction (Figure 1), with no active bleeding. A CT scan revealed esophageal wall thickening without perforation. The patient was kept NPO for 48 hours. Post-procedure, there was no further melena, and hemoglobin levels remained stable.
The patient tolerated a clear liquid diet, which was gradually advanced to regular consistency over two days. She was maintained on PPI twice daily for eight weeks, recovered well, and was discharged in stable condition.
Discussion: This case highlights the critical importance of early recognition and management of acute esophageal necrosis, particularly in patients with severe underlying conditions such as poorly controlled diabetes and sepsis. Despite the initial severe presentation and complications, including significant gastrointestinal bleeding, the patient responded well to conservative management with proton pump inhibitors, dietary modifications, and supportive care. Timely diagnosis via esophagogastroduodenoscopy and appropriate therapeutic interventions played crucial roles in her recovery.
This case underscores the necessity for vigilance in patients presenting with upper gastrointestinal symptoms in the setting of systemic illness, as prompt treatment can significantly improve outcomes in acute esophageal necrosis.
Disclosures:
Jose W. Sotelo, MD1, Akanksha Togra, MD1, John Joyce, MD2, Brian Lee, DO3, Pratyusha TIrumanisetty, MD4. P2300 - Acute Esophageal Necrosis: An Uncommon Culprit Behind Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2SUNY Upstate Medical University, Syracuse, NY; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, San Antonio, TX; 4Memorial Medical Center, El Paso, TX
Introduction: Acute esophageal necrosis (AEN), or "black esophagus," is a rare, serious condition marked by widespread necrosis of the esophageal mucosa. It often presents with upper gastrointestinal bleeding, sepsis, or signs of peripheral hypoperfusion, mainly affecting elderly patients with comorbidities like diabetes, cardiovascular disease, and chronic renal insufficiency. This report details the case of an 80-year-old female with poorly controlled diabetes who developed AEN during septic shock from emphysematous pyelonephritis.
Case Description/Methods: An 80-year-old female with poorly controlled diabetes presented to the Emergency Department in septic shock due to emphysematous pyelonephritis. Admitted to the ICU, she was treated with vasopressors and antibiotics. On the fourth day, she developed coffee-ground emesis and melena, with hemoglobin dropping from 12 g/dL to 7 g/dL. Despite this, she was hemodynamically stable and started on a proton pump inhibitor (PPI).
An esophagogastroduodenoscopy (EGD) showed diffuse esophageal necrosis sparing the gastroesophageal junction (Figure 1), with no active bleeding. A CT scan revealed esophageal wall thickening without perforation. The patient was kept NPO for 48 hours. Post-procedure, there was no further melena, and hemoglobin levels remained stable.
The patient tolerated a clear liquid diet, which was gradually advanced to regular consistency over two days. She was maintained on PPI twice daily for eight weeks, recovered well, and was discharged in stable condition.
Discussion: This case highlights the critical importance of early recognition and management of acute esophageal necrosis, particularly in patients with severe underlying conditions such as poorly controlled diabetes and sepsis. Despite the initial severe presentation and complications, including significant gastrointestinal bleeding, the patient responded well to conservative management with proton pump inhibitors, dietary modifications, and supportive care. Timely diagnosis via esophagogastroduodenoscopy and appropriate therapeutic interventions played crucial roles in her recovery.
This case underscores the necessity for vigilance in patients presenting with upper gastrointestinal symptoms in the setting of systemic illness, as prompt treatment can significantly improve outcomes in acute esophageal necrosis.
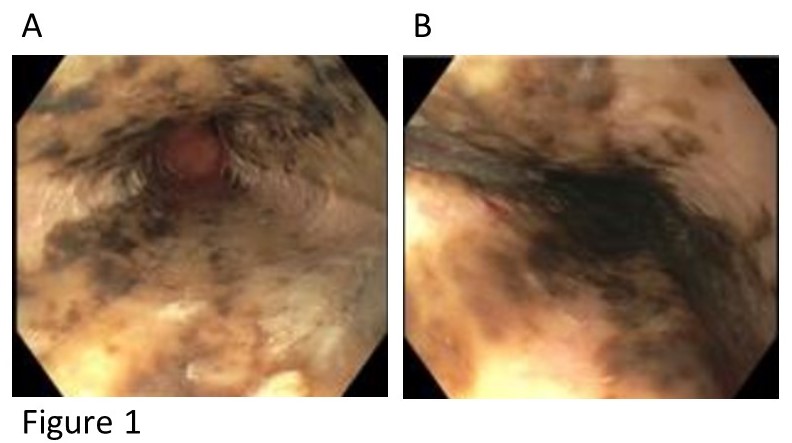
Figure: Figure 1. EGD showing Acute esophageal necrosis
Disclosures:
Jose Sotelo indicated no relevant financial relationships.
Akanksha Togra: Clinexel Inc – Owner/Ownership Interest. Clinexel Life Sciences Pvt Ltd – Owner/Ownership Interest. Cytenet Life science LLP – Owner/Ownership Interest. GLRK Healthcare foundation (Non-profit Organization Company) – Owner/Ownership Interest.
John Joyce indicated no relevant financial relationships.
Brian Lee indicated no relevant financial relationships.
Pratyusha TIrumanisetty indicated no relevant financial relationships.
Jose W. Sotelo, MD1, Akanksha Togra, MD1, John Joyce, MD2, Brian Lee, DO3, Pratyusha TIrumanisetty, MD4. P2300 - Acute Esophageal Necrosis: An Uncommon Culprit Behind Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
