Monday Poster Session
Category: Esophagus
P2328 - A Rare Case of Severe Upper Gastrointestinal Bleeding Due to Esophageal Pseudodiverticulosis in a Patient With CMV Esophagitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Khushbu Patel, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Khushbu Patel, MD1, Jenny Jan, MD2, Elise Roman, MD2, Brooke Glessing, MD3, Gregory Cooper, MD3
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Cytomegalovirus (CMV) esophagitis can lead to the formation of well-demarcated, shallow, and linear ulcers. They rarely progress into deep, cavitary ulcers mimicking pseudodiverticulosis throughout the esophagus. We present a unique case of a patient with human immunodeficiency virus (HIV) and CMV esophagitis presenting with life-threatening upper gastrointestinal (GI) bleeding from extensive esophageal ulcerations mimicking pseudodiverticulosis.
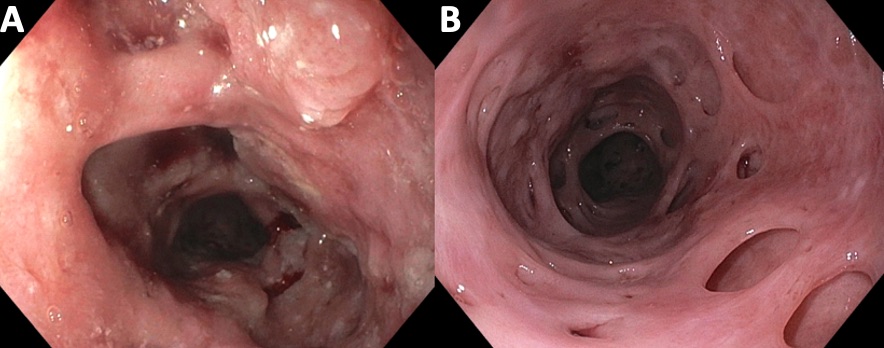
Case Description/Methods: A 53-year-old male with HIV presented with dysphagia, odynophagia, and unintentional weight loss over six months. On exam, he appeared cachectic with significant muscle wasting. Laboratory results revealed CD4 count of 186 cell/mL and viral load 29 copies/mL. EGD showed LA Grade C esophagitis with multiple cratered esophageal ulcers in the upper and middle thirds of the esophagus (Figure A). He was initiated on pantoprazole 40 mg twice a day and discharged. Histopathology from the index EGD resulted following discharge and showed intraepithelial lymphocytes and eosinophils as well as CMV inclusions. Approximately one month later, he presented with multiple episodes of hematemesis and melena. Hemoglobin dropped from 12.2 g/dL to 8.2 g/dL. EGD revealed large amounts of clotted blood with multiple deep pits and cavities suggestive of esophageal pseudodiverticulosis in the whole esophagus (Figure B).
The patient underwent two more EGDs due to ongoing hematemesis, which showed clotted blood and active bleeding from visible vessels within two separate pseudodiverticula. Hemostasis was achieved both times with epinephrine injection and placement of multiple endoscopic clips. The patient was started on IV ganciclovir and discharged with a six-week course of valganciclovir 900 mg twice a day and pantoprazole 40mg twice a day to complete an eight-week course for treatment of CMV esophagitis.
Discussion: Deep “punched out” ulcers or cavitations resembling esophageal pseudodiverticulosis caused by CMV, as seen in this patient, is a rare finding. Despite a low viral load and a CD4 count of >100 cell/mL, this patient developed sequelae of severe CMV esophagitis over a short period of time. Life-threatening hematemesis due to extensive esophageal ulceration from a CMV infection is an uncommon presentation. This case report highlights the importance of considering CMV esophagitis early in patients with pertinent risk factors given the rapid progression and risk of life-threatening bleeding.
Disclosures:
Khushbu Patel, MD1, Jenny Jan, MD2, Elise Roman, MD2, Brooke Glessing, MD3, Gregory Cooper, MD3. P2328 - A Rare Case of Severe Upper Gastrointestinal Bleeding Due to Esophageal Pseudodiverticulosis in a Patient With CMV Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Cytomegalovirus (CMV) esophagitis can lead to the formation of well-demarcated, shallow, and linear ulcers. They rarely progress into deep, cavitary ulcers mimicking pseudodiverticulosis throughout the esophagus. We present a unique case of a patient with human immunodeficiency virus (HIV) and CMV esophagitis presenting with life-threatening upper gastrointestinal (GI) bleeding from extensive esophageal ulcerations mimicking pseudodiverticulosis.
Case Description/Methods: A 53-year-old male with HIV presented with dysphagia, odynophagia, and unintentional weight loss over six months. On exam, he appeared cachectic with significant muscle wasting. Laboratory results revealed CD4 count of 186 cell/mL and viral load 29 copies/mL. EGD showed LA Grade C esophagitis with multiple cratered esophageal ulcers in the upper and middle thirds of the esophagus (Figure A). He was initiated on pantoprazole 40 mg twice a day and discharged. Histopathology from the index EGD resulted following discharge and showed intraepithelial lymphocytes and eosinophils as well as CMV inclusions. Approximately one month later, he presented with multiple episodes of hematemesis and melena. Hemoglobin dropped from 12.2 g/dL to 8.2 g/dL. EGD revealed large amounts of clotted blood with multiple deep pits and cavities suggestive of esophageal pseudodiverticulosis in the whole esophagus (Figure B).
The patient underwent two more EGDs due to ongoing hematemesis, which showed clotted blood and active bleeding from visible vessels within two separate pseudodiverticula. Hemostasis was achieved both times with epinephrine injection and placement of multiple endoscopic clips. The patient was started on IV ganciclovir and discharged with a six-week course of valganciclovir 900 mg twice a day and pantoprazole 40mg twice a day to complete an eight-week course for treatment of CMV esophagitis.
Discussion: Deep “punched out” ulcers or cavitations resembling esophageal pseudodiverticulosis caused by CMV, as seen in this patient, is a rare finding. Despite a low viral load and a CD4 count of >100 cell/mL, this patient developed sequelae of severe CMV esophagitis over a short period of time. Life-threatening hematemesis due to extensive esophageal ulceration from a CMV infection is an uncommon presentation. This case report highlights the importance of considering CMV esophagitis early in patients with pertinent risk factors given the rapid progression and risk of life-threatening bleeding.
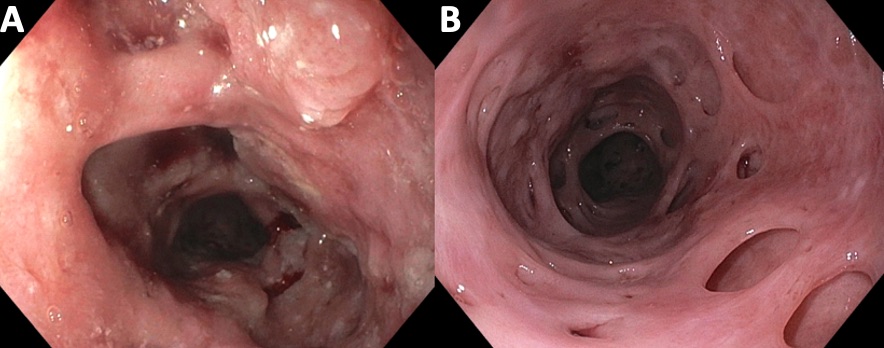
Figure: Figure A. Multiple deep, cratered ulcers in the upper and middle thirds of the esophagus depicting mucosal edema and nodularity. Figure B. Extensive esophageal ulceration consistent with esophageal pseudodiverticulosis revealed throughout the esophagus after removal of clotted blood.
Disclosures:
Khushbu Patel indicated no relevant financial relationships.
Jenny Jan indicated no relevant financial relationships.
Elise Roman indicated no relevant financial relationships.
Brooke Glessing indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Khushbu Patel, MD1, Jenny Jan, MD2, Elise Roman, MD2, Brooke Glessing, MD3, Gregory Cooper, MD3. P2328 - A Rare Case of Severe Upper Gastrointestinal Bleeding Due to Esophageal Pseudodiverticulosis in a Patient With CMV Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

