Monday Poster Session
Category: Functional Bowel Disease
P2330 - Patient Engagement in Community-Based Virtual Gastro Psychology Services for IBS
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tiffany M. Duffing, PhD
GI Psychology
Fairfax Station, VA
Presenting Author(s)
Tiffany M. Duffing, PhD1, Katya Belous, MA2, Emily Singh, MD3, Megan Riehl, 4
1GI Psychology, Fairfax Station, VA; 2Liberty University, Lynchburg, VA; 3Scripps Health, San Diego, CA; 4University of Michigan Health, Ann Arbor, MI
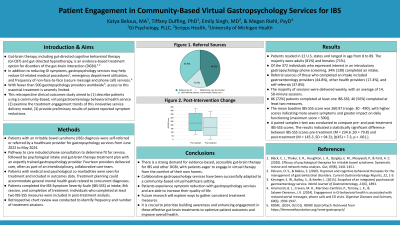
Introduction: To characterize patients utilizing a community-based, virtual gastroenterology behavioral health service and examine the treatment engagement trends of this innovative service delivery model.
Methods: Patients with an irritable bowel syndrome (IBS) diagnosis were self-referred or referred by a healthcare provider for gut-brain therapy from June 2022 to May 2024. Individuals had an introductory screening call to discuss treatment, share symptoms and quality of life, and ask questions.Those appropriate for virtual outpatient gastropsych services participated in a psychological intake with a clinical psychologist or licensed behavioral health clinician. Each of the 14 clinicians who delivered care have expert-level training in gut-brain therapies and participate in weekly group consultation. Clinicians often collaborate with the patients' medical providers. Participants were not excluded from the service or outcomes evaluation when having multiple gastrointestinal diagnoses. Additionally, they were encouraged to integrate general mental health goals and skills related to concurrent diagnoses into their treatment plan. Patients were asked to complete the IBS-Symptom Severity Score (IBS-SSS) at intake, the 8th session, and completion of IBS treatment goals. Individuals who completed at least two IBS-SSS measures were included in outcomes analysis. Retrospective chart review was conducted to identify frequency and number of sessions.
Results: Of the 372 individuals who expressed interest in an introductory phone screening, 32% (120) completed an intake. Referral sources of those who completed an intake included gastroenterology providers (39%), other health providers (23%), and self-referrals (38%). Patients resided in 22 states. The majority were adults (87.15%) and female (68.26%). The majority of sessions were delivered weekly with an average of 14 45-minute sessions. Although 86 (72%) patients completed at least one IBS- SSS, only 27 (23%) completed a subsequent measure. Mean intake IBS-SSS score was 260.97 (range 30 - 490). There was an average 118.75 point (46.55%) decrease in scores among those who completed multiple measures, indicating clinically significant improvement.
Discussion: Patients are interested in engaging in virtual gut-brain therapy from the convenience of their home. There is preliminary evidence that collaborative gastropsychology services can be successfully adapted to a community-based virtual healthcare setting which increases access to evidence-based care.
Disclosures:
Tiffany M. Duffing, PhD1, Katya Belous, MA2, Emily Singh, MD3, Megan Riehl, 4. P2330 - Patient Engagement in Community-Based Virtual Gastro Psychology Services for IBS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1GI Psychology, Fairfax Station, VA; 2Liberty University, Lynchburg, VA; 3Scripps Health, San Diego, CA; 4University of Michigan Health, Ann Arbor, MI
Introduction: To characterize patients utilizing a community-based, virtual gastroenterology behavioral health service and examine the treatment engagement trends of this innovative service delivery model.
Methods: Patients with an irritable bowel syndrome (IBS) diagnosis were self-referred or referred by a healthcare provider for gut-brain therapy from June 2022 to May 2024. Individuals had an introductory screening call to discuss treatment, share symptoms and quality of life, and ask questions.Those appropriate for virtual outpatient gastropsych services participated in a psychological intake with a clinical psychologist or licensed behavioral health clinician. Each of the 14 clinicians who delivered care have expert-level training in gut-brain therapies and participate in weekly group consultation. Clinicians often collaborate with the patients' medical providers. Participants were not excluded from the service or outcomes evaluation when having multiple gastrointestinal diagnoses. Additionally, they were encouraged to integrate general mental health goals and skills related to concurrent diagnoses into their treatment plan. Patients were asked to complete the IBS-Symptom Severity Score (IBS-SSS) at intake, the 8th session, and completion of IBS treatment goals. Individuals who completed at least two IBS-SSS measures were included in outcomes analysis. Retrospective chart review was conducted to identify frequency and number of sessions.
Results: Of the 372 individuals who expressed interest in an introductory phone screening, 32% (120) completed an intake. Referral sources of those who completed an intake included gastroenterology providers (39%), other health providers (23%), and self-referrals (38%). Patients resided in 22 states. The majority were adults (87.15%) and female (68.26%). The majority of sessions were delivered weekly with an average of 14 45-minute sessions. Although 86 (72%) patients completed at least one IBS- SSS, only 27 (23%) completed a subsequent measure. Mean intake IBS-SSS score was 260.97 (range 30 - 490). There was an average 118.75 point (46.55%) decrease in scores among those who completed multiple measures, indicating clinically significant improvement.
Discussion: Patients are interested in engaging in virtual gut-brain therapy from the convenience of their home. There is preliminary evidence that collaborative gastropsychology services can be successfully adapted to a community-based virtual healthcare setting which increases access to evidence-based care.
Disclosures:
Tiffany Duffing: Gastro Girl Digestive Health Insights – Advisory Committee/Board Member. GI Psychology – Employee.
Katya Belous: GI Psychology – Employee.
Emily Singh indicated no relevant financial relationships.
Megan Riehl: GI OnDEMAND – Prior Consultant. GI Psychology – Consultant. Lilly – Consultant. Takada Pharmaceuticals – Consultant.
Tiffany M. Duffing, PhD1, Katya Belous, MA2, Emily Singh, MD3, Megan Riehl, 4. P2330 - Patient Engagement in Community-Based Virtual Gastro Psychology Services for IBS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
